
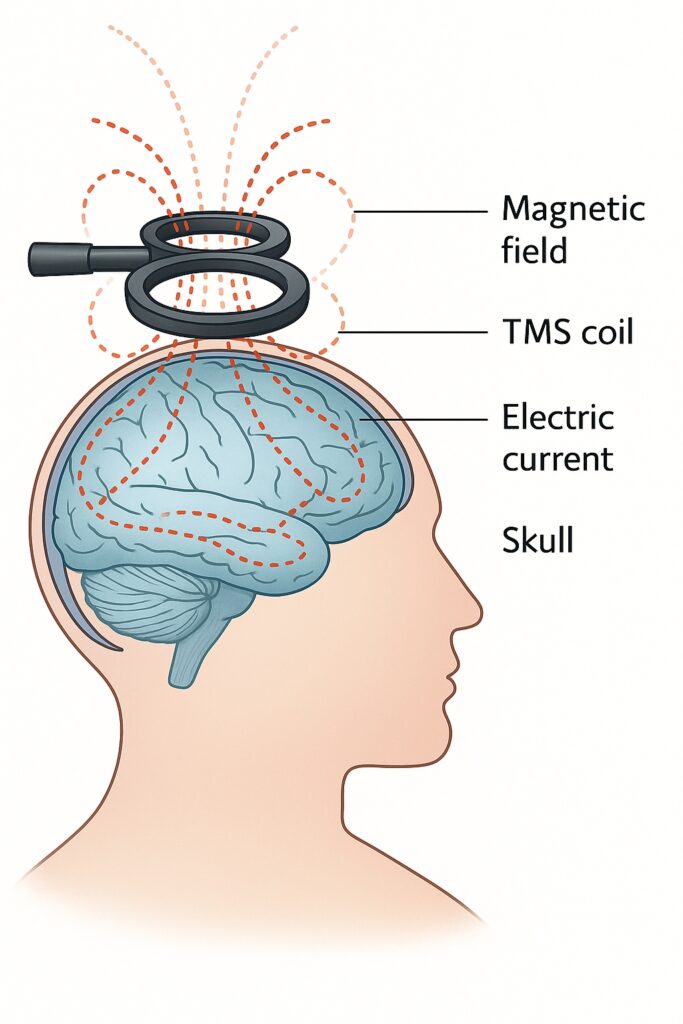
Transcranial Magnetic Stimulation, or TMS, is a non-invasive and painless method used to stimulate or suppress specific areas of the brain using magnetic fields that pass through the skull.
TMS has become a well-established tool in neuroscience and is used in both research and clinical settings. It helps in diagnosing and treating various neurological and psychiatric conditions, such as depression, anxiety, and chronic pain.
The technique can also be combined with other brain imaging methods, such as EEG (electroencephalography) and fMRI (functional magnetic resonance imaging), to better understand how different parts of the brain work and respond to treatment.
History of Transcranial Magnetic Stimulation (TMS)
The idea behind TMS goes back to the 1890s, when the first experiments using magnetic stimulation were carried out in Paris. A French physicist and physician, Jacques-Arsène d’Arsonval, used high-voltage coils and was able to show that magnetic pulses could trigger electrical activity in the brain.
Modern TMS, as we know it today, was developed much later, in 1985, by Professor Anthony Barker and his team at the University of Sheffield. They were building on earlier research from 1980, which used electrical stimulation of the brain’s motor cortex. Although this earlier method (called transcranial electrical stimulation or TES) worked, it was extremely painful. Professor Barker wanted to find a less painful alternative—and this led to the development of the first modern TMS devices. These new devices made it possible to stimulate the brain near the surface of the skull using short magnetic pulses, which are painless and easy to apply.
By the 1990s, physicians began using TMS to treat medical conditions. The first case studies showing positive effects for depression were published in 1993 and 1995. Since then, the method has been proven effective for several psychiatric and neurological conditions.
Today, TMS is officially recognized as a treatment for conditions like depression, OCD, and several neurological illnessess, that haven’t responded to other treatments.
Technical Basics of Transcranial Magnetic Stimulation (TMS)
TMS works based on the principle of electromagnetic induction. This means that a rapidly changing magnetic field is used to create an electric current in the brain. This current stimulates neurons (nerve cells) in a specific area of the brain’s surface.
Here’s how it works in simple terms: A strong burst of energy—between 400 and 2,000 joules—is released through a coil, often shaped like a figure-eight (called a butterfly coil). This energy comes at very high voltage, between 500 and 4,000 Volts, and it creates a magnetic field of up to 3 Tesla (which is very strong). The magnetic field is directed at a right angle to the coil and can pass through the skull without losing much of its strength.
If the electric current in the brain is strong enough to reach the activation threshold of the nerve fibers in the cortex, it triggers a nerve signal. This means that a message is sent through the neurons, just as if the brain had done it on its own.
How TMS Works
A strong burst of energy is released through a coil creating a magnetic field which is directed to a particular brain area
Although not all the details are fully understood, researchers know that transcranial magnetic stimulation (TMS) works by triggering a chain reaction in the brain. When a magnetic pulse is applied from outside the head, it generates electrical activity in nerve cells. This begins with an electrical impulse (called an action potential) that starts in a nerve fiber (axon) and then spreads through the entire nerve cell and its branches (dendrites).
At the same time, other areas of the brain may become less active, possibly due to something called lateral inhibition—where active brain cells suppress activity in neighboring areas. This means TMS doesn’t just activate certain brain regions—it also helps regulate brain activity.
The minimum amount of magnetic force needed to trigger a nerve impulse is called the “stimulation threshold.” This threshold is especially low in sensitive areas like nerve endings or branching points of neurons, making those areas easier to activate.
TMS Treatment
When the primary motor cortex (the brain area responsible for movement) is stimulated, the TMS therapy coil is placed on the scalp directly above it. When the magnetic pulse is released, the person may feel a light tapping sensation on their scalp and hear a clicking sound from the coil. The pulse activates motor neurons, sending a signal down the spinal cord, through motor nerves, and into the muscles. This often results in a small muscle twitch, which can be measured using sensors placed on the skin. At CHMC, transcranial magnetic stimulation therapy in Dubai is used not only for neurological testing but also as an effective treatment option, with transcranial magnetic stimulation helping patients manage depression and other conditions.
As a treatment, TMS does more than just target one spot—it stimulates an entire network of brain regions. This network effect can reach even deeper areas of the brain. Because of this, modern TMS treatment focuses on tailoring the stimulation to each individual’s brain network. The goal is to activate the right brain area, at the right time, to get the best results. This personalized approach is believed to lead to more effective and lasting changes in brain activity.
A typical TMS session lasts between 3 and 30 minutes, and treatment is usually done five days a week for several weeks, depending on the severity of symptoms. Patients remain fully awake and alert, and unlike electroconvulsive therapy (ECT), TMS does not require anesthesia, nor does it cause seizures. This makes it a safer and more comfortable treatment option for many individuals.
Transcranial Magnetic Stimulation (TMS) in Psychiatry
Most people may not be familiar with the dorsolateral prefrontal cortex (DLPFC), but this region plays a critical role in regulating mood and thought processes. It is particularly active in states of rumination—a pattern of repetitive, negative thinking that is one of the core features of depression.
Over the past two decades, medical researchers have turned their focus toward this specific brain region as a target for treatment. Transcranial magnetic stimulation (TMS) is designed to help patients with depression and other psychiatric conditions, especially when traditional treatments like medication and psychotherapy have failed.
TMS in the Treatment of Depression
TMS, especially a specific form called repetitive TMS (rTMS), has been proven to have a significant antidepressant effect. It works by changing the activity in certain parts of the brain that are responsible for mood regulation.
In the United States, the Food and Drug Administration (FDA) approved the first TMS device for this purpose in October 2008. In Germany, TMS was officially included in the national treatment guidelines for unipolar depression in 2015, recognizing its role as a medically accepted treatment option.
TMS has become an established treatment for people with depression that does not improve with medication or therapy alone—also known as treatment-resistant depression. As research continues, the role of TMS in psychiatry is expected to grow, offering a safe and effective alternative for patients in need.
TMS Treatment Session
The most commonly used method targets the left dorsolateral prefrontal cortex—a brain region that tends to be underactive in people with depression. High-frequency rTMS (called HF-rTMS) in this area has been shown in clinical trials to reduce depressive symptoms and, in some cases, even lead to full remission.
A typical TMS treatment plan involves sessions lasting about 20 to 30 minutes, done several times a week over a period of 3 to 6 weeks. Some studies have shown that increasing the number of sessions or the number of magnetic pulses during each session can lead to even better results.
What Makes Transcranial Magnetic Stimulation Different
Although Transcranial Magnetic Stimulation (TMS) and Electroconvulsive therapy (ECT) both stimulate the brain, their approach is very different. ECT involves delivering electrical currents to the brain under general anesthesia to induce seizures, which can rapidly reduce severe depressive symptoms. TMS, on the other hand, modulates brain activity without inducing seizures or requiring sedation. Its safety profile is excellent, with the most common side effects being mild headaches or scalp discomfort. Seizures are extremely rare—estimated at 7 per 100,000 sessions, according to large clinical surveys.
What We Don’t Know about TMS in Psychiatric Treatment
Even though TMS in psychiatric treatment is widely used around the world, there is still no clear agreement on how the treatment should be continued after the initial phase. For example, it’s not yet fully understood how long the benefits last or whether and when booster sessions might be needed.
Also, TMS isn’t placed at a specific point in the overall treatment plan for depression yet, partly because the available research data is still very mixed. Different studies have included very different types of patients, making it harder to compare results and draw clear conclusions.
Still, for many people who have not found relief with other treatments, TMS offers a safe, non-invasive, and effective option to help lift their burden of depression.
Aproved Indications for Transcranial Magnetic Stimulation
Since its first clinical use in 1985 and FDA approval in 2008 for major depressive disorder (MDD), TMS has gained increasing recognition in psychiatry. Apart of depression, TMS is now also FDA-approved for the treatment of:
- Obsessive-compulsive disorder (OCD) – targeting different brain regions involved in repetitive thoughts and behaviors
- Migraine with aura – as a pain management tool
- Smoking cessation – to support addiction treatment efforts
Additionally, ongoing research is exploring TMS for Post-Traumatic Stress Disorder (PTSD), anxiety, and autism spectrum disorders.
Use of Transcranial Magnetic Stimulation (TMS) in Neurology
At first, TMS was mainly used to study how signals travel through the brain’s motor pathways. But over time, it became an important tool in brain research. It helped scientists better understand how the brain works and how different areas are connected. For example, TMS can temporarily “switch off” a small part of the brain so researchers can observe how it affects thinking or movement. It can also show how the brain changes in response to injury or treatment, which has been useful in rehabilitation research.
TMS can also be used as a treatment option for certain neurological conditions such as:
Multiple Sclerosis (MS):
In MS, nerve pathways are damaged by the immune system, affecting movement, coordination, and sensation. TMS can help assess how well nerve signals are traveling and may also support rehabilitation by improving motor function through repeated stimulation.
Parkinson’s Disease:
Parkinson disorder affects movement, causing tremors, stiffness, and slowness. TMS is being used experimentally to improve motor symptoms and reduce depression, which often occurs alongside Parkinson’s. Some studies have shown it may help improve coordination and movement speed.
Stroke:
After a stroke, parts of the brain that control movement or speech can be damaged. TMS can help by stimulating areas of the brain that are still healthy, encouraging them to take over lost functions. It’s being used in stroke rehabilitation to support recovery of movement, especially in the arms and hands.
Tinnitus:
Tinnitus is a constant ringing or noise caused by overactive neuronal activity in the auditory cortex, a part of the brain involved in hearing. TMS is used to calm these overactive brain areas. Some patients have reported relief after repeated sessions, although results can vary.
Migraine:
In people with migraines, TMS can be used during the early phase of an attack to interrupt brain activity linked to the migraine. The U.S. FDA has even approved a portable TMS device for at-home use in migraine treatment.
Epilepsy:
Though TMS can potentially trigger seizures in rare cases, it is also being explored as a treatment for epilepsy. Repeated sessions of TMS, using carefully controlled settings, may help reduce seizure frequency in some patients.
How Transcranial Magnetic Stimulation Helps in Neurology
In all these conditions, TMS can either be used as a diagnostic tool (to test how well brain and nerve circuits are working) or for therapeutic purposes (to help retrain and rebalance brain activity). Because it’s non-invasive and safe, it’s becoming more common in neurology clinics around the world.
While TMS isn’t a cure for neurological disorders, it can be a valuable part of a broader treatment plan—especially for patients who don’t respond well to medication or want to avoid invasive procedures.
TMS Use in Neurological Diagnostics
In neurology, one of the most common uses of Transcranial Magnetic Stimulation is to test how well the connection between the brain’s motor cortex and a specific muscle is working. Along with its role in neurological exams, brain stimulation therapy is also applied in mental health treatment. At CHMC, specialized TMS therapy Dubai programs support patients who do not respond to medication, and TMS for depression has become a proven non-invasive option for improving mood and recovery.
How It Works
TMS can help doctors detect damage in both the central nervous system (like the brain and spinal cord) and the peripheral nervous system (like nerves in the limbs). During this test, a strong magnetic pulse is applied to the scalp above the motor cortex. This pulse causes the brain to send a signal through the motor pathway to a target muscle. The response is measured in the form of a motor evoked potential (MEP)—a small electrical signal that shows how well the message traveled. Doctors usually measure several signals and use the one with the strongest response and fastest arrival time. This gives valuable information about the speed and health of the nerve fibers in the motor pathways.
Also areas further down the spine can be stimulated to tell whether damage is located in the central nervous system or the peripheral nerves. This helps pinpoint exactly where a problem is occurring.
TMS Special Use in Motor Nerve Diseases
This type of diagnostic testing is especially helpful when doctors are trying to diagnose conditions that affect motor nerves, such as multiple sclerosis, ALS, or spinal cord injuries.
TMS as a Precision Medicine Tool
The effectiveness of TMS can be enhanced through personalized treatment approaches. Individual brain imaging (e.g., MRI) helps determine optimal stimulation sites and doses. Advanced methods such as neuronavigation, fMRI imaging, and computer modeling are used to fine-tune TMS parameters and define exact stimulation targets.
To allow simultaneous TMS and fMRI scanning, a specially designed MR receiver coil is placed between the skull and the TMS coil. This setup significantly improves sensitivity, enabling real-time monitoring of brain activity at the stimulation site. Carefully timed TMS pulses ensure compatibility with MRI, allowing safe and accurate assessment of treatment effects.
Non-Invasive Brain Mapping in Neurosurgery
In some advanced neurosurgery centers, TMS is also used to map out important brain areas before surgery, especially for patients with brain tumors. For example, TMS can show exactly where parts of the brain responsible for movement or speech are located—without needing to open the skull. This allows surgeons to remove more of the tumor safely, reducing the risk of damaging vital brain functions and improving long-term outcomes for the patient.
This precision is made possible by combining TMS with high-resolution MRI scans. A special computer system matches the patient’s brain scan with the position of the TMS coil in real time and shows it in 3D. This technique is called “neuronavigated TMS,” and it has become an essential tool in both research and clinical practice.
Side Effects of Transcranial Magnetic Stimulation
Decades of experience across different medical fields have shown that Transcranial Magnetic Stimulation (TMS) is generally safe when used correctly and according to established safety guidelines.
Most Common Side Effects
The most frequent side effects are mild and temporary. These include light headaches and a tingling sensation on the scalp caused by the magnetic pulses. These symptoms usually go away on their own and don’t require treatment. During a TMS session, the clicking sound from the machine can be quite loud—sometimes louder than recommended noise limits. That’s why both patients and medical staff are advised to wear ear protection during the procedure.
Rare but Serious Risks
A very rare but serious side effect is the triggering of an epileptic seizure. Based on data from more than 300,000 TMS sessions between 2012 and 2016, the overall risk of seizure is estimated at 7 out of 100,000 sessions. However, for people with an existing seizure disorder (such as epilepsy), the risk is slightly higher—about 33 out of 100,000 sessions. For these patients, TMS can still be considered but must be used with extra caution.
Who Should Not Get TMS
TMS is not recommended for people who have certain types of implants in or near the brain, such as intracranial electrodes or cochlear implants. These devices can be affected by the magnetic field, which could lead to complications..
Transcranial Magnetic Stimulation (TMS). Summary
Transcranial Magnetic Stimulation (TMS) is a non-invasive technique that uses short magnetic pulses to induce controlled electrical currents in brain tissue. By targeting specific brain regions, TMS allows researchers and clinicians to influence brain activity, making it valuable for both neuroscience research and clinical applications.
TMS helps map language and motor functions in the brain by stimulating various regions and observing behavioral changes. These functional maps are especially useful for planning brain surgeries. Repetitive TMS has also proven effective in treating depression and other psychiatric and neurological disorders.
TMS is a well-tolerated and low-risk procedure for most people. As long as proper precautions are taken—like wearing ear protection and screening for medical conditions—serious side effects are extremely rare.


