
Post-Traumatic Stress Disorder (PTSD) occurs as a delayed psychological reaction to an extremely distressing event, a situation of exceptional threat.
Initially, PTSD and military combat trauma were linked together. Much later psychiatrists recognized that such trauma can be caused by car accidents, plane crashes, natural disasters, domestic violence, or sexual abuse.
The below article describes the diagnostic crieria, rootcauses as well as variety of ptions for treatment of PTSD in Dubai.
Schedule an Appointment with Our Leading Psychiatrist, Dr. Kowal
Call CHMCWhat Is PTSD?
Post-Traumatic Stress Disorder (PTSD) refers to a persistent psychological reaction to a distressing event of exceptional threat or catastrophic magnitude. A trauma, therefore, does not mean difficult life situations such as a separation or the loss of a job, but rather events in which a person’s physical integrity or even life is at risk.
Traumatic experiences may be very brief — for example, a traffic accident or an assault — or they may extend over many years, such as in cases of sexual abuse, political imprisonment, or torture. A characteristic feature of traumatic situations is that those affected are unable to control or actively cope with them. As a result, such events typically trigger profound despair, fear, and helplessness.
Not only those directly affected by such experiences can develop symptoms of PTSD, but also witnesses, close relatives, or individuals who are repeatedly exposed to trauma in their professional roles, such as war photographers, emergency responders, or crisis counselors.
Whether someone subsequently develops PTSD depends on the type and severity of the trauma as well as on additional individual factors.
Historic Note about PTSD
Mankind’s earliest literature tells us that a considerable proportion of military casualties are of psychological nature.
At the end of the First Warld War, a debate about the origin of PTSD arose between Freud’s followers and the military psychiatrists. The first were downplaying the emphasis on the external stimuli causing the “shell shock,” respectively, “battle fatigue,” defending its infantile origins. This explanation turned to be wrong, nevertheless psychoanalysis was the first effective method for the treatment of the “war neurosis.”
The 1952 edition of the DSM-I includes the diagnosis of “Gross Stress Reaction,” which was similar to the modern definition and understanding of PTSD. “Gross Stress Reaction” was defined as a “normal personality utilizing established patterns of reaction to deal with overwhelming fear” as a response to “conditions of great stress.”.
The term “Post-Traumatic Stress Disorder (PTSD)” came into use in the 1970s. The new awoken interest in PTSD was raised as a consequence of the Vietnam War and the high number of traumatized US military veterans.
PTSD was officially recognized as a psychiatric disorder by the American Psychiatric Association in 1980 in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM).
Signs and Symptoms of PTSD
People with PTSD experience feelings of panic or extreme fear linked to the trauma. The most common PTSD symptoms are
- The person relives the traumatic event through intrusive and recurring memories, in particular vivid images and nightmares. Those memories are causing usual intense emotional and physical reactions, such as extreme fears, heart palpitations, sweating, and other somatic symptoms.
- The person is overly alert or wound up, suffering from insomnia, irritability, or lack of concentration.
- The affected individual deliberately avoids activities, places, people, thoughts, or feelings associated with the traumatizing event.
- In the chronic stage of the PTSD, other symptoms, such as loss of interest in day-to-day activities, social detachment, and a feeling of numbness, appear.
The individuals affected by PTSD often develop other mental health problems, most commonly depression, anxiety, and alcohol or drug abuse.
PTSD is a natural response to danger and is almost unavoidable in the short term. In the long term, it possesses self-correcting dynamics, reducing in most of the cases the severity of the symptoms. Only about 20 percent of people exposed to trauma react with long-term (chronic) PTSD.
How PTSD Is Diagnosed
The first step in the diagnostic procedure is taking the patient’s medical history and identifying the symptoms and possible risk factors. In some cases, standardized questionnaires can be used, enabling a structured interview. It’s crucial that the conversation take place in a trusting atmosphere so that the patient can open up and overcome any distrust towards the doctor.
The core of the diagnostic process involves carefully identifying the trauma that caused the disorder and its subjective significance to the individual. Each symptom of PTSD is systematically queried and evaluated in its severity. In addition, other mental health conditions occurring with symptoms similar to PTSD must be ruled out.
Diagnosing PTSD Based on DSM 5
DSM-5 is the diagnostic manual predominantly used in the USA while ICD is the diagnostic manual used by the World Health Organization (WHO). There are only minor differences between DSM-5 and ICD-10 regarding the PTSD criteria.
PTSD can be difficult to diagnose because numerous factors can lead to over-reporting and under-reporting symptoms, dysfunction, and distress. Such statistics manuals as the above-mentioned ICD-10 and DSM-5 provide coherent and standardized diagnostic criteria.
The main criterion for PTSD diagnosis is the persistence of symptoms for more than four weeks. Additionally, the condition should affect functioning in important areas of life. A chronic PTSD will be diagnosed if the symptoms persist for more than three months.
In the chapter below, we present the DSM-5 criteria helpful in identifying PTSD. The DSM-5 diagnostic criteria of the American Psychiatric Association categorize the general criteria for diagnosing PTSD in adults.
Required Symptoms for PTSD Diagnosis
PTSD symptoms generally fall into four main categories:
1. Intrusive Re-Experiencing
- Flashbacks
- Distressing memories
- Nightmares
- Emotional or physical reactions to reminders of the trauma
Patients often describe feeling as if the event is happening again in the present moment.
2. Avoidance
- Avoiding places, conversations, or people linked to the trauma
- Emotional numbness
- Withdrawal from social life
Avoidance may provide short-term relief but usually strengthens the disorder over time.
3. Negative Changes in Thinking and Mood
- Persistent guilt or shame
- Feeling detached from others
- Loss of interest in previously meaningful activities
- Pessimistic or distorted beliefs about oneself or the world
4. Hyperarousal and Reactivity
- Sleep disturbances
- Irritability or anger outbursts
- Difficulty concentrating
- Exaggerated startle response
- Constant feeling of being “on edge”
Symptoms must persist for more than one month and cause significant distress or impairment to meet diagnostic criteria.
How Psychiatrist at CHMC Dubai Diagnoses PTSD
A professional diagnosis is the first step toward healing. Our psychiatrist conducts a thorough assessment that includes:
- Understanding the patient’s symptoms and medical history
- Exploring the traumatic event and its emotional impact
- Using standardized diagnostic tools like structured interviews and questionnaires
- Excluding other potential mental health disorders, which may resemble PTSD in symptoms
To be diagnosed with PTSD, symptoms listed in the paragraph above, such as intrusive memories, nightmares, avoidance behaviors, anxiety, or emotional numbness must persist for more than four weeks and significantly affect daily functioning. If symptoms go beyond three months, the diagnosis shifts to chronic PTSD.
The diagnostic process takes place in a supportive, non-judgmental environment. Creating trust is essential so that the patient can open up about difficult memories without feeling threatened, ashamed, or misunderstood.
Other Mental Healt Disorders Associated with PTSD
It’s not uncommon for people with PTSD to suffer from other mental illnesses. Such conditions may either develop directly as a result of the traumatic event or appear later, following the PTSD.
The most frequent of the co-occurring psychiatric disorders are depression and anxiety, especially when the PTSD has persisted for a long time.
Many people attempt to “treat” their symptoms with alcohol or medication, trying to sleep better or block out intrusive thoughts. However, this approach is ineffective—in fact, over time, it only intensifies emotional distress, cognitive disturbances, and finally an addiction.
Depression and PTSD
Depression is a common mental health problem. In the industrialized countries, depression (mild, moderate, or severe) affects around one in ten individuals per year. The pre-existing depression adds to the risk of developing PTSD, and in reverse, PTSD can trigger depression in previously healthy individuals.
It is a fact that prior to the trauma, people with PTSD are three to five times more likely to suffer from depression. On the other hand, individuals with PTSD are four times more likely to develop depression. PTSD also significantly increases the risk of suicide. The recommended treatment for depression associated with PTSD is the use of antidepressants.
Anxiety and PTSD
The American Psychiatric Association (APA) in the past classified PTSD as an anxiety disorder. Such an association is understandable, as PTSD and anxiety disorders might cause the same symptoms.
The common symptoms occurring in PTSD and in the anxiety disorders are fluctuating anxiety, panic attacks, and insomnia. On the other hand, the pre-existing anxiety disorders increase the risk of PTSD after trauma exposure.
PTSD and Substance Abuse
Mental healthcare providers noted that PTSD and substance abuse often coexist. A summary of several studies has shown that around half of patients suffering from PTSD fulfill the criteria for substance abuse disorders. PTSD and alcohol dependence in traumatized individuals often occur at the same time. The reason for alcohol over drug abuse is because of alcohol’s legal status and its availability.
PTSD Treatment Options
Early and comprehensive treatment by a psychiatrist is essential for overcoming PTSD. In most cases, treatment can be provided on in an outpatient setting. Hospital admission may become necessary if the patient also suffers from severe depressive symptoms, an acute psychosis, or an immediate risk of suicide.
Treatment primarily consists of trauma-focused psychotherapy, with medication added if needed. The goal of an overall treatment plan is to:
- help the patient gain control over intrusive and unwanted memories,
- reduce accompanying symptoms such as anxiety, depression, sleep disturbances, and concentration problems,
- support the patient in integrating the traumatic experience into their life story and finding new meaning in life, and
- improve psychosocial functioning, particularly restoring the ability to work.
Treatment Course at CHMC Dubai
At the beginning of treatment, our therapist will provide detailed information about the condition, whenever possible involving family members or other close persons. In the next step he will propose an appropriate therapy plan.
Within four weeks after the appearance of the symptoms, the use of medication in the therapy for PTSD is not recommended. The treatment of choice for PTSD is psychotherapy.
Once the patient has achieved sufficient emotional stability, the therapist starts the process of graduall confrontation with the traumatic experiences. The PTSD symptom reduction or even healing happens through bringing the unconscious traumatic memories to light.
Trauma-Focused Psychotherapy
TFP is the most effective evidence-based treatment for PTSD. “Trauma-focused” means that treatment focuses on the memory of the traumatic event and their associations.
The three most effective forms of trauma-focused psychotherapy are Eye Movement Desensitization and Reprocessing (EMDR), followed by two cognitive-behavioural therapy techniques: Cognitive Processing Therapy (CPT) and Prolonged Exposure Therapy (PE).
In some cases, especially those resistant to CBT, psychodynamic psychotherapy is indicated.
EMDR—Therapy of Choice for PTSD

Francine Shapiro, an American psychologist, made an important discovery through her personal experience. During a difficult period in her life, shortly after being diagnosed with cancer, she noticed that specific eye movements reduced her anxiety and negative thoughts while walking in nature. This led to the development of EMDR therapy, which has become a therapy of choice for PTSD.
This observation deeply impressed her and led her to integrate these guided eye movements into her therapeutic sessions.
During EMDR therapy, clients are asked to recall their traumatic experiences while following the rapid, rhythmic movements of the therapist’s fingers with their eyes.
How EMDR Helps Brain Reprocess Traumatic Memories
Under normal circumstances, the brain processes experiences and stores them as integrated memories. However, a traumatic event is often too overwhelming to be processed in an organized way. As a result, the memory of the trauma remains stored in an unprocessed, raw form. These fragments often consist of intense sensory impressions, physical sensations, and emotions, indicating the core symptoms of PTSD.
Because these memories are not properly integrated, they can be triggered by any reminder of the traumatic event. For example, someone who was once attacked on the street may suddenly feel terrified and react defensively when hearing footsteps behind them.
EMDR specifically targets this mechanism. Through bilateral stimulation—most commonly eye movements—the brain is guided to reprocess the traumatic memories. This mechanism allows the old, distressing information to be reorganized and integrated into normal memory networks. As a result, maladaptive coping patterns, such as avoidance or overcompensation, can be resolved. Over time, the painful memories lose their intrusive, emotionally charged nature and become neutral, manageable recollections.
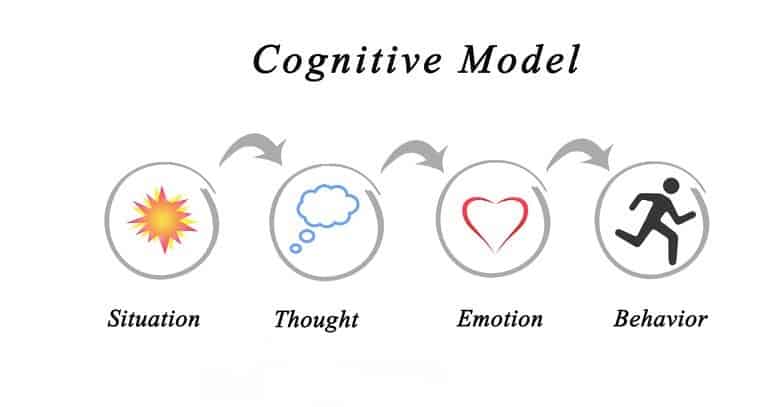
Cognitive Model of CBT (Cognitive-Behavioral Therapy)
Cognitive-behavioural therapy (CBT) is based on the idea that people internally interpret situations, thoughts, and emotions differently. Such misinterpretation activates protective mechanisms that cause patients to act out through avoidance and social isolation.
CBT used in the treatment of PTSD tries to change the way a trauma victim feels and acts by influencing his patterns of thinking and behaviour. It uncovers the negative emotions, helping the individual to identify thoughts and feelings making him feel afraid.
Examples of CBT in Treatment of PTSD
The cognitive-behavioural therapy for PTSD might use exposure therapy, stress-inoculation training, cognitive processing therapy, behavioural activation, acceptance, and commitment therapy.
Many of these therapy methods have demonstrated success in treating the primary problems of PTSD and co-occurring depressive symptoms.
Exposure therapy is a type of cognitive behavioural therapy that involves assisting trauma survivors to re-experience distressing trauma-related memories. The goal is to remind and facilitate habituation and successful emotional processing of those memories. Exposure therapy programs include different techniques. One of them is an imaginary confrontation with the traumatic memories. The other is real-life exposure to trauma reminders.
Prolonged Exposure (PE) in Treatment for PTSD
Prolonged Exposure (PE) therapy involves repetitive talking about the trauma until the memory is no longer a hindrance. This gives the patient more control over his trauma-related thoughts and feelings. It helps to bring the traumatic memories to “the light,” making them conscious and decreasing their destructive effect.
Cognitive Processing Therapy (CPT) for PTSD Treatment
Cognitive Processing Therapy (CPT) belongs to cognitive-behavioural therapy techniques described below. Along with EMDR and PE, CPT is the most effective evidence-based psychotherapy for PTSD. CPT focuses on thoughts and emotions caused by the traumatic events. It builds a bridge between bodily sensations and the associated thoughts and feelings. It helps to understand how the trauma changes feelings, thoughts, and behaviour, relieving the person from the vicious circle triggered by the event.
PTSD Treatment with Psychodynamic Psychotherapy
The CBT it’s the most well-researched PTSD treatment method, but it doesn’t help all patients. In some cases, psychodynamic psychotherapy is the more effective method.
The conducted studies show that psychodynamic psychotherapy can have several benefits. It is more effective for the individuals who were the victims of violence. The other group of patients responding well to psychodynamic psychotherapy are the perpetrators.
Methods of Psychodynamic Psychotherapy in PTSD Treatment
Psychodynamic psychotherapy places a large emphasis on the exploration of the unconscious. Its main approach is uncovering and making conscious the hidden upsetting feelings and thoughts.
Such suppressed and unconscious content influences the patient’s current behaviour. That’s why the psychodynamic psychotherapy focuses not only on the encapsulated trauma content but also on the current conflicts with roots in the past.
Treating PTSD with Interpersonal Group Psychotherapy
Interpersonal Psychotherapy is an effective group therapy treatment for PTSD involving meeting with a group of other people sharing the same or a similar traumatic event.
It is easier to talk about traumatic events with other people who have been through a similar experience. An open trial of interpersonal psychotherapy reported high rates of remission from PTSD symptoms without using exposure.
Treatment with Medication for PTSD

The use of medication for PTSD treatment is not the first method of choice. However, PTSD is frequently associated with other psychiatric diagnoses like depression or anxiety.
The combination of PTSD with other psychiatric disorders requires a more complex therapy plan, including the use of medication.
In such situations, a combination of psychotherapy and pharmacotherapy can improve the positive therapy outcome.
The use of antidepressants can be effective, especially in the treatment of severe and/or residual PTSD and/or coexisting psychiatric comorbidities such as depression. In such cases, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are helpful in reducing the intensity of the PTSD symptoms.
Supportive Treatment for PTSD
Traumatized people frequently feel stigmatized and might avoid seeking professional help. They worry about confidentiality breaches or potential professional repercussions if they disclose their psychological distress.
Social Support in PTSD
Among post-traumatic factors, the extent of social support is the most extensively researched factor. Perceived social support appears to influence the strength of the relationship between trauma severity and PTSD symptoms.
Family Support in Treatment for of PTSD
After a traumatic experience, it’s crucial for the affected individual to be supported by their family members. This includes actively listening and taking the other person’s feelings seriously. Especially in cases of suicidal statements, immediate medical assistance should be sought.
Encourage the affected individual to start therapy and be willing to be involved if the therapist deems it helpful. Accept any support offers yourself so you can better assist and stay healthy at the same time.
Complementary Therapy for PTSD
The overall treatment plan often incorporates creative approaches such as music therapy or art therapy, as well as movement therapy and other methods to improve posture and movement patterns (Feldenkrais, Qi Gong, occupational therapy).
Through relaxation techniques (yoga, autogenic training) or biofeedback, the patient learns to better control their symptoms. If necessary, as part of therapy, the individual receives support for career or social reorientation, grief processing, or relationship issues.
Course of PTSD
The progression of post-traumatic stress disorder (PTSD) varies. Some symptoms may appear during the traumatic event itself or shortly afterward. In some cases, the symptoms surface after a latency period lasting weeks or even months. This delayed onset of symptoms is often observed in soldiers after combat missions.
After the onset of PTSD, the symptoms may subside after a few weeks, while for others, they can persist for many years and even become chronic. Often, phases of milder symptoms alternate with periods of more severe ones.
The prognosis of successful treatment of PTSD has improved in recent years. The long-term prognosis for PTSD is good, and symptoms often disappear or lessen with treatment. Such positive therapeutic effects can be achieved with treatment initiated soon after trauma and with healthy social support. The prognosis is good, especially in high-functioning individuals without pre-traumatic psychiatric disorders. About half of those affected even recover without treatment (spontaneous remission).
Many people manage to overcome and handle the trauma-related memories after a few months. However, for about 30% of those affected, the symptoms persist for at least three years. With appropriate treatment, PTSD typically lasts an average of 3 years, while without therapy, it lasts around twice as long and can get chronic.
Prognosis of PTSD. Is Full Recovery Possible?
With appropriate treatment, many individuals recover fully from PTSD. Approximately half of all PTSD cases improve even without treatment, but professional therapy significantly increases the likelihood and speed of recovery.
With proper treatment, the average recovery time is around three years—but the time frame varies widely depending on the individual’s situation, trauma type, and resources.
Early treatment by a psychiatrist not only reduces suffering but also helps patients rebuild their lives, maintain employment, improve emotional well-being, and strengthen relationships. When untreated, PTSD can become chronic in about 30% of cases and persist for years.
Causes of PTSD

The main factor contributing to the onset of PTSD is the sudden appearance of a severe trauma, which breaks the psychic balance of the affected individual. The quick and massive influx of traumatizing events exceeds the psychological defense, not allowing for the neutralization of the harmful feelings.
Violent traumatic events such as accidents, abuse, and disasters break through the Ego defense mechanisms. As a result, people store traumatic memories in their raw, unprocessed form.
PTSD can develop not only in people directly harmed by trauma but also in those witnessing such events. One of the triggering factors for PTSD in people witnessing such trauma might be the survivor’s guilt. Also, soldiers who killed the enemy can develop PTSD due to the perpetrator’s trauma.
Despite the formative role of the trauma in triggering the onset of PTSD, there are several other factors modulating the development of the condition. One of the most important factors is the neurobiology of the brain, followed by genetic, environmental, and psychosocial factors.
Treatment for PTSD in Dubai. Summary
The history of PTSD is the history of wars, but at the same time, the history of psychology dealing with the war trauma. The modern sciences became aware of the psychological combat damage caused by the traumas of World War I. The first psychological treatment for PTSD during World War I was Freudian psychoanalysis.
The term “Post-Traumatic Stress Disorder (PTSD)” came into use in the 1970s. The new awoken interest in PTSD was raised as a consequence of the Vietnam War and the high number of traumatized US military veterans. PTSD was officially recognized as a psychiatric disorder by the American Psychiatric Association in 1980.
The first step in treatment for PTSD is an in-depth diagnostic procedure such as psychiatric evaluation, physical exam, and laboratory test. In the second step, a thorough psychological interview follows. In some cases, the psychometric testing might be indicated to secure the diagnosis.
The therapy of choice for PTSD is psychotherapy. Typically, treatment can be done in an outpatient setting. The treatment primarily involves trauma-focused psychotherapy, if necessary, with medication support.
Our psychiatric clinic in Dubai offers effective trauma processing methods, including cognitive behavioural therapy (CBT) and eye movement desensitization and reprocessing (EMDR), as well as other techniques.
FAQ (Frequently Asked Questions)
In the below Frequently Asked Questions section, we provide the answers to the most common concerns of our patients about PTSD. Our psychologists are specialized in therapy for PTSD.
What is PTSD?
PTSD, known as Post-Traumatic Stress Disorder, emerges following exposure to or witnessing a traumatic event. It elicits profound and unsettling emotions, thoughts, and responses associated with the trauma.
What Are the Symptoms of PTSD?
PTSD symptoms usually begin shortly after the traumatic event; sometimes they can appear months or years later. Typical for PTSD is when the symptoms persist for more than 4 weeks, causing severe distress and interfering with people’s personal lives. The symptoms can also fluctuate in severity over the years. Symptoms of PTSD:
Re-experiencing symptoms: Memories of the event appearing repeatedly. This can be nightmares or trauma memories (“flashbacks”) related to the event.
Avoidance: The person avoids things reminding him of the trauma. They can avoid places or people related to the event or even suppress talking and thinking about such an event.
Negative feelings and thoughts: After the event, the person experiences negativistic thinking. He might feel numb and unable to express emotions, even towards the loved ones.
Hyperarousal: The hyperarousal is frequently associated with insomnia, lack of focus, and an unhealthy lifestyle such as overeating, excessive smoking, or abusing alcohol or drugs.
Other PTSD symptoms: shattered self-image and worldview, enduring distrust in others, intense guilt, shame, or self-loathing. Performance in significant life areas is impaired, and coping with daily life becomes a struggle.
What types of events can cause PTSD?
PTSD can be triggered by various traumatic events, such as combat exposure, physical or sexual assault, natural disasters, serious accidents, or witnessing a traumatic event happening to others.
How is PTSD diagnosed?
Diagnosis of PTSD involves a thorough evaluation by a qualified mental health professional, which may include a review of symptoms, medical history, and assessment of how the symptoms are impacting daily functioning.
What are the risk factors for developing PTSD?
Risk factors for PTSD include experiencing intense or prolonged trauma, having a history of mental health conditions, lacking a strong support system, experiencing additional stressors after the trauma, and having a family history of PTSD or other mental health disorders.
Is PTSD treatable?
Yes, PTSD is treatable with various forms of therapy, such as cognitive-behavioural therapy (CBT), exposure therapy, eye movement desensitization and reprocessing (EMDR), and medication. Treatment aims to reduce symptoms, improve coping skills, and enhance overall quality of life.
How long does PTSD last?
The duration of PTSD can vary greatly among individuals. Some people may experience symptoms for a few months, while others may struggle with symptoms for years. Early intervention and appropriate treatment can help reduce the duration and severity of symptoms.
Can PTSD go away on its own?
Without treatment, PTSD symptoms may persist or worsen over time. Seeking professional help and participating in therapy can significantly improve outcomes.
I suffer from sleeplessness, mood swings, and the same memories from the past coming repeatedly. Do you think I have PTSD?
PTSD is a mental health problem people develop after being exposed to a life-threatening event or witnessing such an event happening to someone close to them. Sometimes the symptoms occur directly after the trauma, sometimes even years later. Typical for PTSD are memories, called “flashbacks,” insomnia, and anxiety. The diagnosis requires in-depth investigation, which must be done by an experienced psychiatrist or psychologist.
I was involved in a severe car accident…
Later, I developed anxiety and intrusive memories related to the accident. Now I’m scared to drive a car. My GP suspects that I might have PTSD. Can you treat it with medication?
Your GP can be right, but before talking about treatment, the diagnosis of PTSD must be secured. In some cases, PTSD counselling alone can be sufficient. The counselling (psychotherapy) methods used for PTSD treatment are called trauma-focused psychotherapies. The most effective among them is Eye Movement Desensitization and Reprocessing (EMDR)
Are PTSD and borderline personality disorder similar?
PTSD (Post-Traumatic Stress Disorder) and BPD (borderline personality disorder) share some similarities, such as emotional dysregulation and difficulties in relationships. However, they are distinct conditions with different underlying causes and diagnostic criteria. PTSD typically develops in response to a traumatic event, while BPD involves pervasive patterns of instability in self-image, relationships, and emotions.
Are PTSD and trauma the same?
PTSD (Post-Traumatic Stress Disorder) and trauma are distinct concepts. Trauma signifies an event or experience that profoundly disturbs or distresses an individual, often surpassing their coping abilities. In contrast, PTSD is a mental health disorder that may arise following exposure to or witnessing such traumatic events. While trauma can precede PTSD development, not all individuals who experience trauma will develop PTSD.
Can PTSD cause memory loss?
Yes, PTSD (Post-Traumatic Stress Disorder) can cause memory problems, including memory loss or difficulty recalling specific details of the traumatic event. This can occur due to the intrusive nature of traumatic memories as well as the impact of stress hormones on memory encoding and retrieval processes.
Why do PTSD patients relive trauma?
Individuals with PTSD frequently experience trauma re-experiencing through intrusive memories or flashbacks. These vivid and distressing recollections of the traumatic event can be triggered by various cues or reminders. These memories can be triggered by reminders of the trauma, such as sights, sounds, or smells, and can feel as though the event is happening again in the present moment. This re-experiencing of the trauma is a hallmark symptom of PTSD and can lead to significant distress and impairment in daily life.
How can I recognize that I have PTSD?
After a trauma, people might develop upsetting memories, called “flashbacks,” and feel easily irritable. It is a fact that other symptoms typical for PTSD are insomnia, anxiety, and depression. PTSD affects your social and professional activities like going to work, being effective at work, seeing friends, and enjoying the social interactions. Some people develop PTSD symptoms immediately after the trauma. By others, the symptoms may come over time. If the symptoms and thoughts related to the trauma persist over months, upsetting you and causing problems in your life, it’s likely that you have PTSD.
Who can develop PTSD?
Another PTSD fact is that anyone can develop PTSD at any age. Several factors make people more likely to get PTSD, most of which are beyond the person’s control. For example, an intense or prolonged traumatic event makes a person more likely to develop PTSD. Also, personal factors such as previous traumatic experiences, age, and gender can influence the risk for PTSD.


