
Schizophrenia is a serious mental disorder characterized by profound impairments in thinking and feeling. Schizophrenia does not mean “split personality.” Rather, it describes a state in which the mind loses its usual connection with reality causing confusion and distress for the affected individuals and their families.
In most patients, especially those untreated, schizophrenia develops progressively. The end stage of such dynamics is the residual schizophrenia characterized by major personality changes and the patient’s invalidism.
In this article, we will explore treatment for schizophrenia in Dubai and the options available for those seeking help.
Schedule an Appointment with Our Leading Psychiatrist, Dr. Kowal
Call CHMCPsychosis and Schizophrenia
The term psychosis refers to various mental disorders characterized by changes in thinking, feelings, and people’s perceptions of themselves and the world around them. Schizophrenia is the most common disorder within the wider group of psychosis.
Schizophrenia affects people from all walks of life. The most frequent onset of schizophrenia happens in younger people age between 15 and 30, both men and women alike.
Etymology and Terminology
The word “schizophrenia” comes from the Greek roots “schizo” = division and “phrene” = spirit, describing the fragmented thinking of people with this disorder.
Swiss psychiatrist Eugen Bleuler coined the term “schizophrenia.” Despite the term’s meaning, schizophrenia does not imply “split mind.” Public opinion frequently confuses schizophrenia with dissociative identity disorder, also known as “multiple personality disorder” or “split personality disorder,” a rare psychiatric condition.
Signs and Symptoms of Schizophrenia
Psychiatrists characterize the symptoms of schizophrenia as “positive” or “negative.” Symptoms caused by the disease (e.g., hallucinations, delusions) are labeled “positive.” “Negative” symptoms refer to traits that have been lost through illness (e.g., drive and motivation have disappeared). In most cases, the patient denies his illness and refuses to seek professional help. Other symptoms include:
Jumbled thinking
People with schizophrenia may have trouble getting their thoughts straight. This often means that a person says things that don’t make sense to others.
Disorganized thinking and speech
Such disorganization may range from loss of train of thought to loosely connected sentences up to the full incoherence known as “word salad.”
False, unshakable beliefs
Paranoia (beliefs of persecution): the person may believe that others are trying to harm him.
Ideas of grandeur
The patient believes that he has strange powers or is omnipotent.
Altered sense of self
The person has a strange perception of his body; he may feel his arms and legs, or other parts of his body, do not belong to him or are altered. Sometimes he feels like he is bodiless and nonexistent as a person. He finds it difficult to distinguish between where his body stops and where the rest of the world begins.
Thoughts broadcasting
The patient is convinced that others can hear his thoughts or that the TV or radio is sending him special messages.
Hallucinations
Most frequent are auditory hallucinations, such as hearing voices.
Changes in emotions
Emotions may get dull and flat or out of control and overexcited. Flattened emotions may result in a lack of facial expression and an inability to maintain normal social interaction. The emotions may also be incongruent to the situation, for example, laughing at some sad news or crying at something funny.
Loss of purpose
The person feels drained of energy and drive, losing interest in life. The progression of the illness causes the neglect of his health and personal hygiene.
Social withdrawal
The person retreats from the world, avoids the company of others, and isolates himself, losing social skills and not being able to survive on his own in his society. Most people with schizophrenia do not have all these symptoms. These symptoms affect some individuals more severely than others.
How does schizophrenia develop?
Any human thought, perception, and reaction, including the appropriate evaluation of others’ behaviour and the ability to establish trusting contacts, are the products of complex brain functions.
The undisturbed chemical balance of neurotransmitters in the brain ensures the proper processing of environmental stimuli and inner psychological thought circuits. This forms the basis of attention, organized thinking, and purposeful actions.
The disturbance of various metabolic processes in the nerve cells in different brain regions causes the symptoms of schizophrenia. The dopamine neurotransmitter system is affected, along with the glutamatergic or GABAergic excitatory transmission.
Remarkably, schizophrenia is also linked causally to genes that control the early developmental organ formation of the brain and ensure the formation of neural networks.
Causes of schizophrenia
There are several assumptions about why the neurotransmitters involved in the central nervous system become imbalanced. However, no one knows yet what causes schizophrenia. The most plausible explanation is the multifactorial origin of schizophrenia. Genetics, early environment, neurobiology, and psychological and social processes appear to be important contributory factors.
Genetics
Historically, Kraepelin and Bleuler, the pioneers in the identification and treatment of schizophrenia, were in favour of the hereditary cause of schizophrenia. Bleuler wrote, “Schizophrenia appears to be independent of external conditions and circumstances.”
Kraepelin also emphasized the genetic (inheritance) factor, adding it as a potential cause of physical illnesses in childhood, such as brain inflammation.
Vulnerability to schizophrenia is partly inherited, with no single gene responsible for the condition. The illness is more likely to occur in those with a schizophrenic first-degree relative in the general population. Nevertheless, the majority of individuals with a close blood relative with schizophrenia do not develop the illness themselves. And schizophrenia commonly occurs in families where no one is known to have had the illness before.
Birth complications or infectious diseases of the nervous system are also discussed as causes of schizophrenia.
Neurobiology
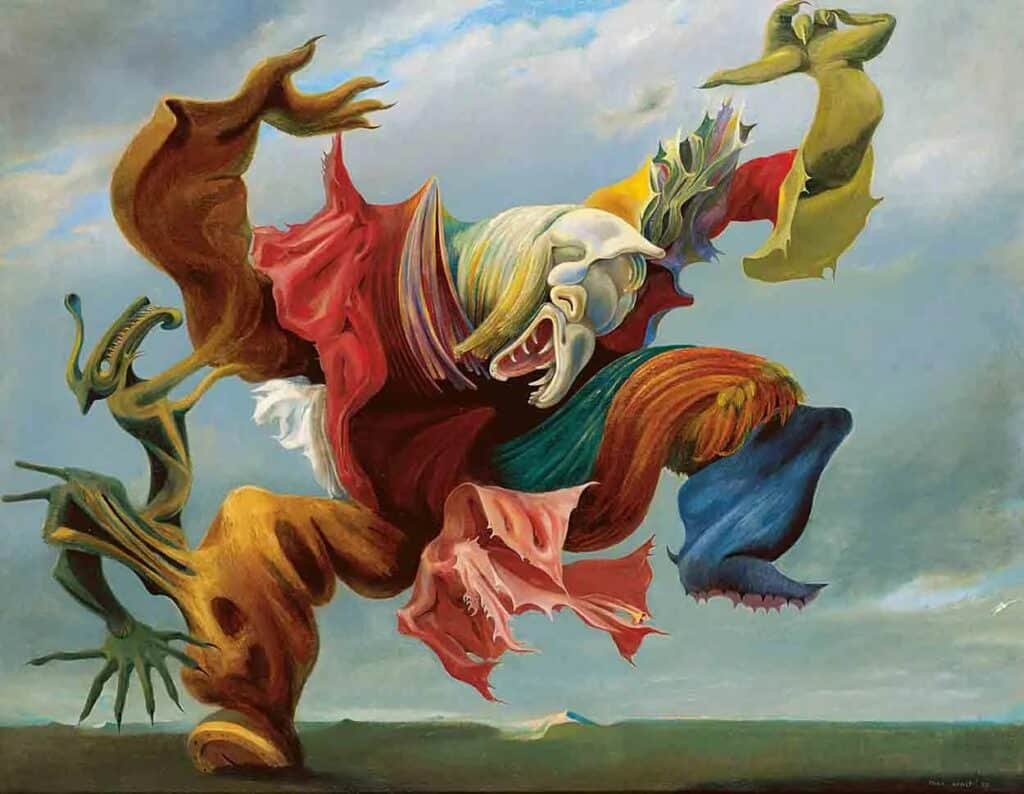
Current research is focused on the role of neurobiology. There are billions of nerve cells in the brain. Each nerve cell has branches, which transmit and receive messages from other nerve cells. The branches release chemicals called neurotransmitters, which carry the message from the end of one nerve branch to the end of another. In the brain afflicted with schizophrenia, something goes wrong in this communication system. The evidence that schizophrenia is a biologically based disease of the brain has accumulated rapidly during the past two decades. Dynamic brain imaging systems have recently supported this evidence. This image precisely shows the wave of tissue destruction that takes place in the brains of the sufferers.
Environmental factors
Recently, research proved the role of environmental factors in the onset of schizophrenia. Several studies have examined the relationship between experience of a stressful event during pregnancy and later psychosis. The study concluded that children of mothers exposed to sudden disasters during pregnancy have an increased risk of schizophrenia.
Also, stressful events in childhood, such as broken homes or child abuse, correlate with a higher risk for schizophrenia. Such events are seen as triggering factors for schizophrenia in vulnerable individuals. These events can also modify or exacerbate the course of the illness once it has developed.
Early and regular use of psychoactive substances such as THC, methamphetamine, opiates, and hallucinogenic drugs increases the risk for psychosis.
An increased prevalence of psychosis in urban compared to rural settings is one of the recent consistent findings in schizophrenia research. In a recent follow-up study of the entire Swedish population, those living in the urban areas had around 70% higher risk of developing schizophrenia compared to the rural population.
Also, social isolation and social disadvantage, such as low social class, reduced access to health care, lack of social support, unemployment, and poor physical health, correlate with increasing the risk for schizophrenia.
Types of schizophrenia
There are diverse types of schizophrenia with varying impacts on the patient’s thinking content, feelings, and behaviours.
Since Bleuler‘s time, the definition of schizophrenia has continued to change. The main achievement was the more accurate differentiation of the distinct types of schizophrenia.
Without knowing the exact causes of schizophrenia, the classification is based on the appearance of symptoms occurring together. The most common symptoms of schizophrenia are delusional thinking, hallucination, emotional indifference, and social withdrawal.
The classification, in accordance with ICD-10, a diagnostic system of the World Health Organization (WHO), distinguished the following types of schizophrenia:
Paranoid Schizophrenia
It is the most common type of schizophrenia in most parts of the world. Relatively stable, frequently paranoid delusions, typically accompanied by auditory hallucinations and perceptual disturbances, dominate the clinical picture.
Hebephrenic or Disorganized Schizophrenia
In hebephrenia, also called disorganized schizophrenia, the predominant symptoms are affective changes, followed by fragmentary delusions and hallucinations, erratic behaviour, and mannerisms. The mood is shallow and inappropriate and often accompanied by giggling or self-absorbed smiling, or by a lofty manner, grimaces, mannerisms, pranks, hypochondriacal complaints, and reiterated phrases. Thought is disorganized, and speech is rambling and incoherent. There is a tendency to remain solitary, and behaviours seem empty of purpose and feeling. This form of schizophrenia usually starts between the ages of 15 and 25 years and tends to have a poor prognosis because of the rapid development of “negative” symptoms, particularly the flattening of affect and loss of volition.
Catatonic Schizophrenia
Catatonic schizophrenia, one of the classical types of schizophrenia, has become extremely rare in Western and industrialized nations. This subtype is marked by distinct psychomotor disturbances, often alternating between extremes such as stupor and excessive motor activity (hyperkinesis), or between automatic obedience and extreme negativism. Patients may maintain rigid postures or unusual movements for long periods, and sudden episodes of violent excitement can also occur.
Though its exact cause remains unclear, catatonic schizophrenia is still more frequently observed in developing regions. These motor symptoms may be accompanied by a dreamlike or oneiroid state, in which the person experiences vivid scenic hallucinations. While it shares some positive symptoms of schizophrenia, such as hallucinations and agitation, it may also progress into residual schizophrenia, where the more dramatic symptoms fade but emotional and social withdrawal persist.
Schizophrenia Simplex (Simple Schizophrenia)
Schizophrenia simplex is a less common form of the disorder, but it still appears in industrialized countries like the UAE. This subtype is marked by a slow, progressive decline in social and occupational functioning. Unlike paranoid schizophrenia, it typically lacks clear delusions and hallucinations, making it harder to diagnose. Instead, the condition manifests through negative symptoms such as emotional blunting, lack of motivation, and social withdrawal.
The condition may gradually lead to social impoverishment and behaviors like vagrancy, as the person becomes increasingly detached from daily life. This “silent implosion” of personality often results in a decline that can mimic residual schizophrenia over time. Early recognition and intervention are vital. Those experiencing such symptoms should consider schizophrenia treatment in Dubai, where care options include therapy, medication, and long-term support. Seeking help from the best psychiatrist in Dubai or getting admitted to a specialized psychiatric hospital in Dubai can ensure a comprehensive and compassionate treatment plan.
Residual Schizophrenia
This type is a chronic stage in the development of schizophrenia. It is the end stage of an auto-destructive brain process that happens on the neurobiological level and leads to permanent changes of the brai structure. On the psychological level, it’s characterized by the “negative” symptoms combined with severe intellectual and emotional impairment and progressing invalidism.
The Two Faces of Schizophrenia
Symptoms of schizophrenia are often divided into two main categories—positive and negative symptoms.
Positive symptoms
Positive symptoms are misleadingly named. They are disturbing experiences that aren’t part of normal perception. People may see or hear things that aren’t there (hallucinations) or hold strong beliefs that do not match reality (delusions). They may feel watched, guided, or controlled by external forces, or speak in ways that are difficult to follow. These experiences can be frightening but are part of the illness, not a reflection of the person’s character.
Negative symptoms
On the other hand, negative symptoms involve a loss of emotional expression or motivation. The person might withdraw from social contacts, show little facial expression, or lose interest in daily activities. They may struggle to feel joy, express affection, or engage with others. These symptoms can persist for longer and often make recovery more challenging.
In children and adolescents, early signs can appear as delayed development, social anxiety, poor school performance, or preferring to play alone rather than with others.
Treatment for Schizophrenia in Dubai
To achieve the best results in the treatment for schizophrenia is the proper care to the patient. This implies early recognition and treatment at the earliest stage of the disorder. The therapy of choice for schizophrenia is always treatment with medication.
Antipsychotic medication plays a crucial role in treating schizophrenia. By using this medication, we can suppress, and ideally even fully eradicate, the symptoms of schizophrenia.
The prerequisite of an effective treatment is close psychiatric monitoring and the use of psychotherapy. Other crucial roles in the treatment of schizophrenia include the involvement of social workers, education, and family integration. The next step is the patient’s integration into society, for example, through a protected work environment and/or the patient’s professional education, helping him to find a suitable occupation and get financial independence.
Prophylaxis includes training of the primary health care personnel, allowing the recognition of the early signs of schizophrenia. The other measure is providing public education to decrease stigma and discrimination against people with mental health disorders.
Treatment Options for Schizophrenia at CHMC Dubai
Modern psychiatry offers many effective ways to manage schizophrenia. The treatment plan at CHMC combines medical therapy, psychotherapy, and psychosocial support, adapted to each individual’s needs and phase of illness. Some patients begin with inpatient stabilization, while others are treated in outpatient settings under close supervision.
Therapy with Medication for Schizophrenia
During acute phases, our psychiatrist prescribes so-called antipsychotic medication, which helps regulate brain chemicals such as dopamine and serotonin. Antipsychotics reduce delusions, hallucinations, and confused thinking.
Modern second-generation medications like risperidone, olanzapine, quetiapine, or aripiprazole are preferred for their effectiveness and lower risk of side effects.
Improvement usually appears gradually, often within several weeks. Once symptoms decrease, our psychiatrist carefully adjusts the dose to a maintenance level that helps prevent relapse.
Stopping medication without supervision is risky and often leads to symptom recurrence, so continuous follow-up with a psychiatrist in Dubai for treatment of schizophrenia is essential.
At CHMC, we monitor each patient closely, ensuring that the medication is well-tolerated, effective, and adjusted to personal needs. We also emphasize trust and cooperation—because a good therapeutic relationship is the foundation of patient’s compliance and recovery.
Psychotherapy and Psychoeducation for Patients with Schizophrenia
Once the acute symptoms are under control, psychotherapy plays a vital role. It helps patients understand their condition, process difficult experiences, and rebuild self-confidence. Individual and group therapy sessions teach coping strategies and stress management.
Psychoeducation is another important part of treatment. Our therapists provide clear information about the illness, the importance of medication, and ways to recognize early warning signs. We highly encourage family sessions as they foster understanding and alleviate tension at home. When relatives know what to expect, they can provide stronger and more supportive care.
Social and Occupational Rehabilitation
Healing from schizophrenia also means rebuilding life skills. Social therapy programs help patients return to daily routines, work, and social participation. Occupational therapy, structured day programs, and lifestyle guidance support reintegration into community life.
The involvement of family and friends is key. A stable, understanding environment significantly reduces the risk of relapse.
Cognitive Rehabilitation for Patients with Schizophrenia
Even after hallucinations and delusions fade, some people experience difficulties with concentration, memory, and problem-solving. Cognitive rehabilitation for patients with schizophrenia at CHMC helps train these functions using structured exercises. Improved cognitive abilities support better self-awareness, medication adherence, and the ability to manage daily tasks effectively.
Living with Schizophrenia
Schizophrenia is a long-term condition, but with the right care and consistency, recovery is possible. Treatment is not just about controlling symptoms—it’s about helping people rebuild their confidence, relationships, and purpose.
Our team focuses on restoring balance, emotional stability, and quality of life through compassionate, individualized therapy. Many of our patients in Dubai return to work, education, and fulfilling social lives with ongoing psychiatric and psychotherapeutic support.
Psychiatric Treatment of Schizophrenia in Dubai. Summary
Schizophrenia is a serious yet manageable mental health condition. Our psychiatrist at CHMC in Dubai offers the treatment for schizophrenia, emphasizing early diagnosis and a tailored therapy plan.
The treatment for schizophrenia includes medication, psychotherapy, and family education. With proper care and consistency, most individuals diagnosed with schizophrenia can recover, regaining balance and independence.
At CHMC—Clinic for Health and Medical Care in Dubai, we follow the highest German standards in psychiatry. Our multilingual team is dedicated to providing compassionate, evidence-based treatment for people struggling with schizophrenia and related mental health conditions.
Facts about Schizophrenia in Bullet Points
- Schizophrenia affects about 24 million people worldwide, which makes up 1% of the global population.
- It is a treatable disorder. There are effective interventions (pharmacological and psychosocial) available.
- The earlier the treatment begins, the more effective it will be.
- More than 50% of persons with schizophrenia are not receiving appropriate care
- 90% of people with untreated schizophrenia are in developing countries
- Care of persons with schizophrenia can be provided at community level, with active family and community involvement
FAQs about Schizophrenia
In the below FAQ section, we summarized answers to the common question asked by our patients about eating disorders.
What is schizophrenia?
Schizophrenia is a serious mental health condition that affects how a person thinks, feels, and behaves. People with schizophrenia may have trouble distinguishing between reality and imagination, often experiencing hallucinations, delusions, and disorganized thinking.
What causes schizophrenia?
Schizophrenia is thought to be caused by a mix of genetic, biological, and environmental factors. It runs in families, but stress, trauma, or drug use can also contribute to its development.
Is schizophrenia the same as having multiple personalities?
No, schizophrenia is not the same as dissociative identity disorder (multiple personality disorder). Schizophrenia affects perception and thinking, not personality.
Can schizophrenia be cured?
There is no cure for schizophrenia, but it can be managed effectively with medications, therapy, and a strong support system. Many people lead fulfilling lives with proper treatment.
What are common symptoms of schizophrenia?
Common symptoms include:
- Hallucinations (hearing or seeing things that aren’t there)
- Delusions (strong beliefs not based in reality)
- Disorganized thinking
- Lack of motivation or emotional expression
Who is at risk of developing schizophrenia?
Schizophrenia can affect anyone, but it often appears in late teens to early 30s. Men may develop symptoms slightly earlier than women.
Can stress make schizophrenia worse?
Yes, stress can worsen symptoms or trigger a relapse. A calm, supportive environment can help reduce stress and improve outcomes for those with schizophrenia.
Are people with schizophrenia dangerous?
Most people with schizophrenia are not violent. With treatment, they are no more likely to harm others than the general population. Misunderstanding the illness often fuels this stereotype.
How is schizophrenia diagnosed?
Schizophrenia is diagnosed through medical history, psychiatric evaluation, and ruling out other conditions. It requires at least six months of symptoms, with one month of active symptoms like hallucinations or delusions.
Can someone with schizophrenia live a normal life?
With the right treatment and support, many people with schizophrenia can work, maintain relationships, and enjoy a good quality of life.
What are the early warning signs of schizophrenia?
Early warning signs can include social withdrawal, unusual or paranoid thoughts, trouble concentrating, changes in sleep patterns, and a lack of motivation or emotional expression. These symptoms may appear gradually before more severe symptoms develop.
How do antipsychotic medications work, and what are their side effects?
Antipsychotic medications help reduce symptoms by balancing chemicals in the brain, such as dopamine. Common side effects can include drowsiness, weight gain, dry mouth, and sometimes movement issues like tremors. Newer medications often have fewer side effects.
How can family members support someone with schizophrenia?
Families can support loved ones by learning about the condition, being patient, encouraging treatment, and creating a stable, stress-free environment. Joining support groups can also help family members better understand how to help.
What role does therapy play in managing schizophrenia?
Therapy, especially cognitive-behavioral therapy (CBT), helps individuals manage symptoms, understand their thoughts and behaviors, and improve problem-solving skills. Therapy can also aid in social skills development and coping with stress.
Are there lifestyle changes that can help reduce symptoms?
Yes, regular exercise, a healthy diet, good sleep hygiene, avoiding drugs and alcohol, and stress management techniques like mindfulness or meditation can all help reduce symptoms and improve overall well-being.
How do hallucinations differ from delusions?
Hallucinations involve sensing things that aren’t real, like hearing voices or seeing things. Delusions are false beliefs that persist despite evidence to the contrary, such as believing one has special powers or is being watched.
Is schizophrenia more common in certain populations?
Schizophrenia occurs worldwide regardless of race, ethnicity, or socioeconomic status. However, factors like poverty and poor access to healthcare can negatively affect diagnosis and treatment rates.
Can schizophrenia go into remission?
Yes, with effective treatment, many people experience periods of remission where symptoms are significantly reduced or absent. Regular treatment and early intervention increase the chances of remission.
What resources are available for people with schizophrenia and their families?
Resources include:
- Mental health professionals (psychiatrists, therapists, social workers)
- Support groups like NAMI (National Alliance on Mental Illness)
- Crisis hotlines and community mental health centers
- Educational programs on mental health and caregiving
- Government and nonprofit organizations offering financial and housing assistance
Learn More About Psychoses and Schizophrenia
- What Causes Schizophrenia
- Psychoses
- Delusional Disorder
- Post Partum Psychosis
- History of Psychoses. From Antiquity to Eugenics
Famous people diagnosed with schizophrenia
A recent Nobel Laureate in Economics, John Forbes Nash Jr., has a lifetime history of schizophrenia. His biography has been documented in the book “A Beautiful Mind” and the Academy Award-winning movie of the same name.
Following is a list of other famous people who have been diagnosed with schizophrenia or who have suffered from schizophrenia:
Albert Einstein`s son, Eduard Einstein
Dr. James Watson`s son (Dr. Watson who co-discovered the structure of DNA and Nobel Prize winner)
Peter Green, Guitarist for the band Fleetwood Mac
Syd Barrett of the band Pink Floyd
Mary Todd Lincoln, wife of Abraham Lincoln (past-President of the United States)


