
We have known for a long time that adequate sleep is essential for our physical and mental well-being. Sleeplessness, also called insomnia, is a symptom with different root causes, such as psychiatric, neurological, or physical. Insomnia erodes our physical and mental well-being. Treating insomnia is important to have a good night’s sleep to improve an individual’s health and quality of life.
Schedule an Appointment with Our Leading Psychiatrist, Dr. Kowal
Call CHMCMany people have a few sleepless nights here and there due to circumstantial life challenges, such as stress or excitement. Such temporary sleep disturbances turn in a few days back to normal. However, if, despite practicing good sleep hygiene and a lack of environmental triggers, people suffer from difficulties falling or staying asleep, there could be an underlying sleep disorder.
In the articles below, we describe various sleep disorders and their root causes, with a special emphasis on the treatment for sleeplessness.
Research on Circadian Sleep Rhythm
To facilitate good all-around health and well-being, it is important to avoid the disruption of the circadian rhythm of sleep. If you cannot get your well-needed 7 to 8 hours of sleep, you might be suffering from insomnia. Insomnia takes on many forms. Some people have trouble falling asleep, staying asleep, or consistently waking too early. In the mental health field, psychologists, counsellors, and psychiatrists know that depressed and anxious patients have trouble sleeping. Another common reason for insomnia is that people have gotten into undesirable personal habits. These habits disrupt their ability to sleep normally. A psychologist, for instance, can analyze behaviours and guide the patient to better sleep. Whatever the reasons, treating your insomnia is an option.
Sleeplessness in Dubai. The “24-hour Society”

Modern life is an overtired life. In the big megacities around the globe, likewise in Dubai, on average, one out of three people experience problems staying asleep. One in five says they always sleep “pretty poorly.” The problem lies in the lifestyle called “24-hour society.”
Sleep is a natural process vital for body and mind; it happens on its own. Normally. Unfortunately, it doesn’t always go smoothly for every third adult. People whose sleep is delicate, like others’ stomachs or heads. It is plausible that the number of individuals with sleep disorders increases as many of the causes contributing to the sleeplessness have also increased.
For example, the dense sensory overload to which most people are now exposed. The artificial light now emanates not only from lamps but also from screens of all sizes. It is the “24-hour society” in which you can stream movies, book flights, and discuss in internet forums at any time.
Sleep Deficit and Its Impact
According to the National Institutes of Health (NIH Publication No. 11-5271), the most common sleep disorder is insomnia. “Chronic insomnia is defined as having symptoms at least 3 nights per week for more than 1 month,” says the NIH. Most cases of chronic insomnia are secondary, which means they are due to other disorders.
According to research done at the Stanford Centre for Sleep Sciences and Medicine, the vast majority of people do not get the sleep they require. In our hectic world, many individuals are developing a sleep deficit. The average hours of healthy sleep per night are between 7 and 9 hours. Most people feel their best when they get 8 hours of sleep.
Over time, being short on sleep causes psychological and physical deficits. The psychological impairments include fatigue, lack of focus, and reduced ability to make proper decisions. In the long run, stress combined with sleeplessness causes burnout, depression, and anxiety.
Not getting enough sleep increases the risk of car accidents, impacts work performance, and affects one’s mood and relationships. Lack of sleep impacts the body as well. Sleeplessness triggers the realization of “fight and flight” hormones such as adrenaline and corticosteroids. Being in such “overdrive” for years is the root cause of civilization diseases like hypertension, diabetes, arteriosclerosis, heart attacks, strokes, and more.
However, the biggest percentage of sleep disorders is caused by psychiatric, physical, or neurological conditions.
Diagnosis of Sleeplessness (Insomnia)
Sleeplessness is often not a disorder in itself but rather a secondary symptom of an underlying psychiatric, neurological, or physical illness. Effective insomnia treatment should therefore focus on addressing the root cause whether psychiatric, physical, or neurological.
Insomnia may occur temporarily during acute stress situations, such as family conflicts or exams, and typically resolves without the need for medical intervention. However, if it becomes chronic, professional evaluation is essential. Diagnostic tools like polysomnography can help identify the cause of persistent sleep issues. In more complex cases, visiting a specialized sleep clinic in Dubai can provide comprehensive care, including therapies often used in narcolepsy treatment and other sleep-related conditions.
Chronic sleep disturbances, however, are a serious health problem. Their frequency and impact on daily life (such as daytime fatigue, increased risk of accidents, and depression) are underestimated. In recent years, the possibilities for diagnosis and therapy have significantly improved. Sleep medicine deals with sleep, the natural physiological changes of the body during sleep, and with disorders affecting the natural restorative function of sleep.
Sleep disorders often require an interdisciplinary approach. In this case, a psychiatrist, psychologist, neurologist, pulmonologist, ENT, and other specialists will work together to diagnose and treat a sleep disorder.
Sleeplessness Caused by Psychiatric Disorders
There are long-standing sleep disturbances that are not attributable to a physical illness. Sometimes unfavourable work circumstances, such as shift work or persistent nocturnal noise, are the root cause. Work and personal worries often cause temporary sleep disturbances that resolve once the stressor diminishes. However, if private and professional stressors persist or sleep disturbances endure, seeking evaluation and treatment is advisable.
The sleep environment significantly influences sleep quality, with factors such as noise, light conditions, and room temperature playing crucial roles. Certain behaviours, like irregular sleep schedules, shift work, and consuming large meals before bedtime, can also adversely affect sleep.
Psychiatric disorders accompany more than half of all sleep disturbances. Severe forms of these disorders commonly entail difficulties in falling and staying asleep or feeling unrefreshed during the day.
Sleeplessness in Depression
Patients with depression, for instance, frequently experience early morning awakenings, complicating their ability to return to sleep. Therapy of insomnia in depression focuses on treatment of depression, for example, with antidepressants. In the middle term, even using an antidepressant in the morning will regulate the sleep.
Sleeplessness in Bipolar Disorder
Bipolar disorder is characterized by mood swings between two extremities, mania and depression. In bipolar disorder, sleeplessness is one of the leading symptoms of mania; it is also associated with bipolar depression.
Sleeplessness and Anxiety
Anxiety disorders significantly disrupt falling asleep, while dementia patients may undergo substantial shifts in sleep patterns, sometimes sleeping excessively during the day and remaining awake at night. A successful treatment of anxiety will remove sleeplessness as one of the symptoms. In the short term, anti-anxiety medication like benzodiazepines can be used; in the middle term, the use of antidepressants as monotherapy is sufficient.
Sleeplessness and Substance Abuse
Substance abuse, notably alcohol and drug dependency, can lead to various sleep disturbances, with severe sleep disruptions often persisting even after discontinuation of the triggering substances.
Sleeplessness Caused by Physical Illnessess
There are various physical illnesses associated with chronic insomnia:
- Severe dysfunction of the liver and kidneys,
- Circulatory disorders of the brain,
- Hormonal disorders, i.e. thyroid dysfunction,
- Chronic inflammatory processes like rheumatoid arthritis
- Asthma,
- Chronic pain,
- Cancer
- Various prescribed and over-the-counter medications
- Alcohol
Neurological Causes of Sleeplessness
Conditions affecting the brainstem, like idiopathic hypersomnia or narcolepsy, can lead to excessive daytime sleepiness. Other neurological disorders with an impact on sleep are Parkinson’s or Alzheimer’s disease, multiple sclerosis, epilepsy, narcolepsy, and stroke.
Nighttime movement disorders, such as restless legs syndrome and nocturnal movement disorders, including sleepwalking, interfere with falling asleep and disrupt sleep continuity.
Another neurological disorder causing insomnia is
Sleep Apnea
Snoring combined with sleeplessness can signal a condition known as sleep apnoea. Nocturnal breathing disorders affect approximately 2 to 5% of the population, with snoring being a common warning sign. Those who snore often experience breathing interruptions during sleep, called apnoeas, which lower blood oxygen levels.
The most common type, obstructive sleep apnoea, occurs when the airway collapses due to muscle relaxation or anatomical factors. These repeated interruptions fragment sleep and trigger stress responses, increasing the risk of cardiovascular and metabolic diseases. Surprisingly, many individuals remain unaware of these disturbances and only notice excessive daytime fatigue.
Diagnosis often requires a sleep study in Dubai, where a sleep specialist uses advanced tools to assess sleep quality. Comprehensive care and therapies are available through sleep medicine in Dubai, including effective options for sleep apnea treatment in Dubai.
Sleep apnoea is the most common respiratory sleep disorder, which is characterized by pauses in breathing. An apneic episode usually lasts 10–30 seconds and reoccurs several times throughout the night. The disorder affects both children and adults.
The following article describes diverse types of sleep apnea. It helps to identify its symptoms and to understand diagnostic approaches and currently used treatment techniques.
Types of Sleep Apnea
Below we describe diverse types of sleep apnea. It helps to identify its symptoms and to understand diagnostic approaches and currently used treatment techniques.
Obstructive Sleep Apnea (OSA)
The first and most prevalent type of apnoea is Obstructive Sleep Apnoea (OSA). This type of apnoea is caused by collapse of the throat muscles or by structural abnormalities of the respiratory tract. According to the National Sleep Foundation, obstructive sleep apnoea is the most common primary respiratory sleep disorder. It affects around 10-30% of adults. OSA is especially dominant in overweight middle-aged men but also postmenopausal women. Structural abnormalities of the respiratory system, e.g., adenotonsillar hyperplasia (overgrowth of the tonsils), are the most common OSA cause in children.
Risk factors for Obstructive Sleep Apnea (OSA)
OSA runs frequently in the families. Other risk factors are old age, obesity, and male gender. Other risk factors are family history, hormonal abnormalities, frequent alcohol use, or smoking. Also, frequent alcohol use, smoking, or regular intake of narcotic painkillers adds to the risk.
Furthermore, OSA occurs more commonly in patients with specific anatomical features, including a larger tongue, an overbite, or excessive soft tissue around the neck. These features can weigh down and obstruct the airway when a person is lying down.
Central Sleep Apnea (CSA)
Only about 1% of the population presents with the second type of apnoea, called Central Sleep Apnoea (CSA). It occurs when the drive to breathe decreases periodically or ceases due to impaired function of the respiratory center. CSA can be classified into non-hypercapnic and hypercapnic.
Hypercapnic CSA is based on hypoventilation, triggered by central nervous system diseases like trauma or stroke. The other cause could be neurological disorders, like myasthenia gravis, and chronic use of certain drugs like opioids (e.g., morphine). The non-hypercapnic type is characterized by a periodic breathing pattern that may be idiopathic (i.e., unclear cause) or caused by heart failure. Some patients receiving PAP treatment for obstructive sleep apnoea develop symptoms of central sleep apnoea. This phenomenon is called “treatment-emergent” or “complex sleep apnoea.”.
Risk factors for CSA are similar to those of OSA. Additionally, patients with a previous stroke or brain tumors, as well as heart disorders like atrial fibrillation, are especially at risk.
Mixed Sleep Apnoea
Finally, a combination of OSA and CSA is sleep apnea. It is often referred to as treatment-emergent or complex sleep apnoea, as described earlier in the text.
Complications of Sleep Apnea

The most common symptom of all apnoea types is severe sleeplessness and consequently daytime fatigue and sleepiness. At night, interrupted sleep can trigger nocturia and stress-induced insomnia. The effects of the disturbed sleep cycles are also apparent during the day because the loss of restful sleep leads to difficulty concentrating, morning headaches, and fatigue.
Individuals with sleep apnoea have an increased risk for cardiovascular and metabolic disorders. All types of sleep apnoea share similar symptoms, although patients with central sleep apnoea usually do not display the same level of snoring as patients with obstructive sleep apnoea do. Sleep apnoea on its own is rarely fatal, but if undiagnosed, it increases the risk for cardiovascular and metabolic disorders. Drops in oxygen levels during the apneic phases can trigger anginal chest pain and irritate heart cells, leading to arrhythmias. Hypertension, coronary artery disease, stroke, and respiratory failure are also more common in apneic patients. Emerging data also suggest that the presence and severity of OSA and associated nocturnal hypoxaemia are associated with an increased risk of type 2 diabetes and cancer.
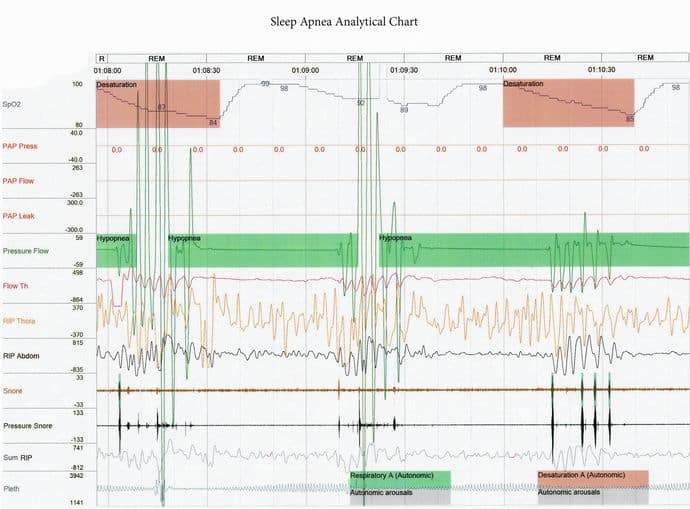
Diagnosing Sleep Apnea
Diagnosing sleep apnoea requires a detailed evaluation of the patient by taking sleep history, including third-party reports. Additionally, a full overnight sleep study in a sleep laboratory is the standard test for individuals in whom sleep apnoea is considered. It usually involves getting monitored overnight with a polysomnogram (PSG). Polysomnography tracks sleep variables like brain function, oxygen and carbon dioxide blood levels, vital signs, and outward symptoms like snoring and movement.
Another variable included in a polysomnogram is the AHI, which is defined as the sum of apnoea’s and hypopneas per hour of sleep. Apnoea is defined as the absence of airflow for ≥ 10 seconds and hypopnea as a reduction in respiratory effort with ≥ 4% oxygen desaturation. An AHI of more than five events per hour of sleep is considered abnormal, and the patient is suspected to have a sleep disorder. An abnormal AHI in combination with excessive daytime sleepiness is characteristic for patients with sleep apnoea.
Assessing Sleep Apnea in Sleep Laboratories
Ambulatory sleep medicine diagnostics involve assessing sleep quality by recording breathing, blood oxygen saturation, pulse, and other parameters overnight. This examination can be done on an outpatient basis, meaning at your home and in your familiar environment. If there are specific questions or indications of disorders, further diagnostics in a stationary sleep laboratory may be necessary.
Treatment for Sleep Apnea
85% of individuals with sleep apnoea go undiagnosed. From those diagnosed, only a low percentage get treated. The treatment approach varies between obstructive, central, and mixed sleep apnoea.
The first step in treating obstructive sleep apnoea is to adopt healthy lifestyle changes. These include losing weight, regular physical activity, quitting smoking and alcohol, avoiding sedatives, and maintaining healthy sleeping habits. It is recommended to sleep on the side instead of on the back to create better airflow into the lungs. In addition to conservative treatment methods, orofacial therapy is advised. It comprises exercises that improve the position of the tongue and strengthen muscles controlling the lips, upper airway, and face.
Continuous Positive Airway Pressure (PAP) Machines
The first-line conservative treatment for obstructive as well as central sleep apnoea is the use of a positive airway pressure (PAP) device. This machine forces the airways open with a stream of pressurized air delivered through a plastic facemask or nasal prongs.
There are three types of PAP devices used for sleep apnoea.
Continuous Positive Airway Pressure (CPAP)
provides a steady stream of pressurized air, and the amount of pressure is the same on inhalation as well as exhalation.
Bilevel Positive Airway Pressure (BiPAP)
delivers two air pressure levels, one for inhalation and another for exhalation, making it easier for the patient to breathe out.
Auto-Adjusting Positive Airway Pressure (APAP)
Auto-Adjusting Positive Airway Pressure (APAP) adjusts the air pressure level based on the patients’ breathing patterns.

Continuous Positive Airway Pressure devices are usually tried first in apnoeic patients, but if not effective, switching to BiPAP or APAP is advised.
CPAP has been shown to significantly improve REM sleep phases, providing healthy, restorative sleep. Ideally, CPAP compliance should take place for as long as the patient is sleeping, but, in practice, this occurs in a minority of subjects.
Observational studies have shown a significant decrease in the risk for stroke and heart disease and lower blood glucose levels in patients being treated with CPAP continuously. However, based on several studies, the average compliance is only about 4 hours per night. Many people eventually stop using it, finding it annoying or difficult to wear, and the problem persists.
Other Treatment Methods for Sleep Apnoea
Patients who are unable to tolerate CPAP treatment or suffer from a milder form of sleep apnoea may benefit from oral mouthpieces, called oral appliances. Oral appliances are custom-made devices that keep the airway open and can be worn at night or throughout the day, depending on the device. Mandibular repositioning or tongue-retaining devices are recommended to be worn at night. A new FDA-approved device, called eXciteOSA, is worn for 6 weeks, 20 minutes a day. It stimulates the tongue muscle with electric impulses to strengthen it and keep it from collapsing during the night.
In some cases, obstructive sleep apnoea can be managed surgically. One approach is to dilate the upper airway by removing structures like the adenoids or realigning the jawbone.

Another possibility is to cause neurostimulation of upper airway muscles by placing implants. The only FDA-approved implantable device is the Inspire Upper Airway Stimulation System. IUASS is placed in the patient’s thorax, monitoring during sleep the respiration. Every time the patient tries to breathe, the device stimulates the hypoglossal nerve, sending a signal to the tongue muscles. The muscles contract, preventing the blockage of the airways.
Treatment for Sleeplessness at CHMC in Dubai
At our Clinic for Psychiatry and Psychology in Dubai, we can assess and treat insomnia. Our professional team will be able to address the mental health aspect of insomnia and determine if depression or anxiety plays a role. In such a case, the available treatment options are medication and psychotherapy/counselling. In case the insomnia doesn’t have a psychological background, we will refer the patients to other specialists.
Treatment of Sleeplessness with CBT at CHMC
The proven psychotherapy method for treating chronic insomnia is Cognitive Behavioural Therapy (CBT), with its benefits lasting long after therapy concludes. Therefore, experts often recommend CBT as the initial treatment for adults.
CBT can be delivered in person or online and consists of various components. Patients learn relaxation techniques and receive guidance on improving sleep habits. Additionally, they learn strategies to break negative thought patterns.
Treatment of Sleeplessness with Medication at CHMC
If CBT is ineffective or not feasible, our psychiatrist will assess the patient and prescribe medication. Sleeplessness is one of the leading symptoms of such psychiatric disorders as depression or anxiety. Benzodiazepines with sleep-inducing effects can be used in the short horizon. The most effective treatment of insomnia in the context of psychiatric disorders is the treatment of the root cause. For example, treating depression and anxiety with antidepressants taken in the morning will regulate the sleep after 4-6 weeks.
Other Treatment Approaches for Sleeplessness
Other treatment options include mindfulness, acupuncture, aromatherapy, exercise, homeopathy, light therapy, massage, meditation, music therapy, or yoga. However, their effectiveness has not been sufficiently supported by studies.
What Can I Do Myself to Get a Better Sleep?
- Create a sleep schedule by going to bed and rising at the same time each day (including the weekend).
- Take care to have a bedroom that is quiet, dark, relaxing, and at a comfortable temperature.
- Assure your bed is very comfortable and that it is only used for sleep and intimacy. (Leave your gadgets and TV in the common living space.)
- Agree on a time during the day to discuss and resolve issues.
- Avoid eating heavy meals too late in the day.
- Nap carefully. Napping in the afternoon for more than 60 minutes can disrupt overnight sleep.
- Exercise as often as possible, but not too close to bedtime.
- Avoid drinking alcohol, as it interferes with getting excellent quality sleep.
- If you consume caffeinated drinks (tea, coffee, energy drinks, etc.), keep in mind that caffeine can remain in your body for up to 14 hours.
- Use the last hour of your waking time relaxing in a dimly lit space.
- Don’t use alcoholic drinks as a “sleep aid.”.
Treatment of Sleeplessness. Summary
Sleep disorders are among the most common health problems, affecting one-third of the adult population in Western countries. Insomnia occurs when individuals experience insufficient or non-restorative sleep. The majority of those affected have difficulty falling asleep (sleep onset insomnia), staying asleep (sleep maintenance insomnia), or both. The clinical picture of insomnia also includes symptoms such as excessive daytime sleepiness as well as sleepwalking or talking in sleep (parasomnia).
Primary insomnia, characterized by severe sleep disturbances with physical or psychiatric roots, requires treatment.
Circadian Sleep Rhythm
The circadian sleep rhythm is the “inner clock” that regulates sleep in all mammals, including humans. This inner clock serves the function of dividing the day into natural rhythms for sleep and being awake. This “master clock” is located in the brain part called the hypothalamus. Like a fine-tuned sensor, the hypothalamus receives ongoing information about light, temperatures, and food consumption, and it adjusts the body accordingly. When everything runs smoothly, people sleep and feel well.
Sleep Apnea
Sleep apnoea is a common sleep disorder that, in around 85% of the cases, goes undiagnosed.
In Central Sleep Apnoea (CSA), treatment should mainly focus on the underlying internal medicine or neurological disorder.
In Obstructive Sleep Apnoea (OSA) Continuous Positive Airway Pressure (CPAP) devices can be used. If CPAP treatment isn’t effective, patients with central sleep apnoea (CSA) may benefit from supplemental oxygen during the night. In cases of a symptom’s persistence, switching from Continuous Positive Airway Pressure (CPAP) to Bilevel Positive Airway Pressure (BiPAP) or Auto-Adjusting Positive Airway Pressure (APAP) is recommended.
Treatment of Sleeplessness with Medication
Our psychiatrist can do a mental health assessment and treat underlying disorders like depression and anxiety. When indicated, he prescribes medications to address the underlying psychiatric disorders causing insomnia. The most effective treatment of sleeplessness in the context of psychiatric disorders is treatment with antidepressants. Even if they are taken in the morning, antidepressants will regulate the sleep after 4-6 weeks.
Treatment of Sleeplessness with Psychotherapy (Counselling)
Many individuals in Dubai report that they feel just fine on 5 or 6 hours of sleep or can cope with sleepless nights. They feel they can catch up on the weekend and vacations. The reality, however, is that we cannot catch up on the physical and mental health benefits, so if you cannot sleep, it will behove you to seek treatment for your insomnia. The psychotherapy treatment method of choice for insomnia is Cognitive Behavioural Therapy (CBT). The therapy helps uncover underlying causes of poor sleep. These can range from poor sleep hygiene to deeper concerns about life.
Our clinic offers diagnostics and treatment of the sleep disorders caused by psychiatric conditions, which account for up to 50% of sleep disturbances.
FAQ’s Related to Sleeplessness (Insomnia)
In the below Frequently Asked Questions section, we provide the answers to the most common concerns of our patients about insomnia.
We are specialised in the therapy of psychiatric disorders; among them, we also treat insomnia.
For more information, contact CHMC, German Clinic for Psychiatry and Psychology in Dubai: +971 4 4574240
What is sleeplessness?
Sleeplessness, also known as insomnia, refers to difficulty falling asleep, staying asleep, or experiencing restful sleep despite having the opportunity to do so.
What are the common causes of sleeplessness?
Common causes of sleeplessness include stress, anxiety, depression, irregular sleep schedules, poor sleep habits (e.g., excessive screen time before bed), medical conditions, certain medications, and environmental factors.
How can sleeplessness affect my health?
Sleep deprivation can result in various health complications, including daytime fatigue, irritability, concentration difficulties, memory impairment, weakened immune function, heightened accident risk, and increased susceptibility to chronic conditions like obesity, diabetes, and heart disease. Moreover, insufficient sleep is a primary symptom associated with mental health disorders.
What are the symptoms of sleeplessness?
Signs of sleeplessness comprise challenges in falling asleep, frequent awakenings throughout the night, premature waking in the morning, lack of feeling refreshed upon waking, daytime fatigue, irritability, trouble concentrating, and mood swings.
How is sleeplessness diagnosed?
The diagnosis of sleeplessness typically involves a thorough evaluation of sleep patterns, medical history, and lifestyle factors. Your doctor may also conduct physical exams and recommend sleep studies if necessary to identify underlying sleep disorders.
What are some tips for improving sleep quality?
Strategies for enhancing sleep quality encompass adhering to a regular sleep schedule, establishing a calming bedtime ritual, cultivating a comfortable sleep environment, moderating caffeine and alcohol consumption, engaging in regular physical activity, managing stress, and refraining from heavy meals near bedtime.
When should I see a doctor about my sleeplessness?
You should consider seeing a doctor if sleeplessness persists for more than a few weeks, significantly impacts your daily functioning, or is accompanied by other concerning symptoms such as chronic pain, difficulty breathing, or persistent anxiety or depression.
What are the treatment options for sleeplessness?
Treatment options for sleeplessness may include cognitive-behavioural therapy for insomnia (CBT-I), prescribed sleep medications, addressing underlying medical or mental health conditions, and making lifestyle modifications to promote better sleep.
Can certain medications or lifestyle factors contribute to sleeplessness?
Yes, certain medications, such as stimulants, antidepressants, and corticosteroids, can contribute to sleeplessness. Lifestyle factors like irregular sleep schedules, excessive screen time, poor diet, and lack of physical activity can also disrupt sleep.
Can sleeplessness cause dizziness?
Yes, sleeplessness can potentially lead to dizziness. Lack of sleep can disrupt the body’s normal functioning, including balance mechanisms, which may contribute to feelings of dizziness or lightheadedness. Additionally, sleep deprivation can affect cognitive function and coordination, further increasing the risk of experiencing dizziness.
Can sleeplessness cause high blood pressure?
Yes, sleeplessness or chronic insomnia can potentially contribute to high blood pressure over time. Lack of adequate sleep can lead to increased stress hormones, such as cortisol, and disrupt the body’s natural processes that regulate blood pressure. Additionally, sleep deprivation can negatively impact blood vessel function and increase inflammation, both of which are risk factors for hypertension. Therefore, addressing sleeplessness and improving sleep quality may be important for overall cardiovascular health and blood pressure management.
How does sleeplessness affect mental health?
Sleeplessness can have a profound impact on mental health, contributing to mood disturbances, cognitive impairments, increased stress, and decreased quality of life. Addressing sleep issues is essential for maintaining mental well-being.
I developed sleeplessness…
The sleeping tablets from my GP don’t help anymore. Since a few weeks I must drink wine to fall asleep. Can you help me?
Sleep deprivation is one of the first symptoms of disturbed psychological balance. Eventually symptoms of depression and/or anxiety will appear. That alcohol is not a suitable substance to treat sleeplessness. Its regular intake will lead to dependency. Taking into consideration your circumstances, a psychiatric consultation would be highly recommendable.
It takes me up to 3 hours to fall asleep…
Panadol night doesn’t work anymore. My GP advised me to visit a psychiatrist. Can counselling help?
Sleep deprivation (problems to fall asleep or difficulties in maintaining the sleep), especially lasting longer than a few days, are very frequently the first symptoms of depression, anxiety, bipolar disorder, or other psychiatric condition. Sleeplessness can also be caused by some physical illnesses. We recommend visiting first a psychiatrist. The first step in diagnosing insomnia is the exclusion of physical problems. If such sleeping tablets as Panadol night do’t help, most probably you will need a proper psychiatric medication. In cases of underlying depression or anxiety, medication should be combined with counselling.
My wife noticed that I’m getting breathing brakes while sleeping. Do you think that I have sleep apnoea?
Your description sounds like you might have sleep apnea. However, the diagnosis must be first secured. The standard investigation for sleep apnoea is ENT examination and then sleep studies in a so-called sleep laboratory. In some cases, sleep apnoea can be caused by a physical block in the nose or throat. Sometimes its root cause might be the malfunction of a particular area in the brain responsible for sleep regulation. Based on the examination results, you will know: 1.) if you need treatment 2.) and if so, which method should be used.
Do you treat sleep apnoea?
Sleeplessness can be misinterpreted as sleep apnea. Sleeplessness is one of the leading symptoms of depression and anxiety. We don’t treat sleep apnoea at CHMC but can do the preliminary diagnostics and, if needed, refer you to a sleep laboratory.


