
The antidepressants address the entire spectrum of depressive symptoms, improving mood and energy, reducing anxiety, and regulating sleep. Depending on the type, antidepressants have different profiles. Some of them have more mood-enhancing and anti-anxiety effects, while others work more stimulatingly.
The effect of antidepressants evolves over weeks. The patient doesn’t feel any causal connection between their intake and the resulting effect. Therefore, the antidepressants are not addictive.
The antidepressants are most commonly used for treatment of depression. However, due to their anxiety-reducing effect, they are also prescribed for anxiety disorders such as phobias, generalized anxiety disorder and panic attacks. Other uses for antidepressants include eating disorders, OCD, PTSD, and depression in bipolar disorder.
For treatment of depression, contact our specialists at CHMC in Dubai
Call CHMCRead more about depression:
- Treatment for Depression
- Self-Assessment Test for Depression
- Post Partum Depression
- Major Depressive Disorder. Diagnosis and Treatment
- Dysthymia. Diagnosis and Treatment
- Catatonic Depression. Diagnosis and Treatment
- Premenstrual Dysphoric Disorder (PMDD)
- Relaxation Techniques in Therapy for Depression
- Helping Family Members with Depression
- Psychotherapy for Older Adults with Depression
- From Early Understanding to Modern Diagnosis of Depression
- Antidepressants. What They Are
- Feeling Depressed? Effects of Loneliness and Social Isolation
Antidepressants. Historical Note
Antidepressants were developed in the late 1950s. In the early 1950s, during drug trials for tuberculosis, researchers observed unexpected mood improvements in patients treated with Iproniazid. This medication works by inhibiting the Monoamine Oxidase (MAO) enzyme, which breaks down neurotransmitters like norepinephrine, serotonin, and dopamine. As a result, these neurotransmitters accumulate in the synaptic gap, improving mood. Although Iproniazid was approved for depression in 1958, it was withdrawn later due to serious side effects.The first effective and well-tolerated antidepressant was Imipramine, introduced in 1957, belonging to the group of tricyclic antidepressants. While effective, these are now rarely used due to their more pronounced side effects compared to newer options. Today, those seeking safe and effective depression treatment in Dubai often consult a qualified psychiatrist in Dubai or visit a reputable mental health clinic in Dubai for updated therapy and medication guidance.
SSRIs and SNRIs
The first modern antidepressant, and the first of the class called Selective Serotonin Reuptake Inhibitor (SSRI), was Fluoxetine. It was discovered by Eli Lilly Company in 1972, and after intense clinical studies, it was approved in 1986.
The second modern antidepressant, Venlafaxine, which belongs to the Serotonin–Norepinephrine Reuptake Inhibitor (SNRI) group, was introduced to the US market in 1993. Venlafaxine blocks the reuptake of serotonin and noradrenaline. In comparison to other antidepressants, Venlafaxine acts faster, mostly due to norepinephrine reuptake inhibition.
Benefits and Risks of Antidepressants

Antidepressants need in average 3 to 4 weeks to develop the full efficacy. Most of the antidepressants have an initially stimulating effect followed by mood improvement, increased energy level, and reduction of anxiety. The initial overstimulation might be dangerous for patients experiencing severe depression or anxiety. It can “backfire,” increasing anxiety or triggering suicidal thoughts. Thus, the choice and the treatment with antidepressants should be monitored by an experienced psychiatrist.
Antidepressants do not induce euphoria. They are only effective in people with depression. Antidepressants work as a kind of scaffolding, maintaining a patient’s psychological balance. After restoring the patient’s functionality, he/she has the means to implement life changes. Although antidepressants are effective in the short and medium term, long-term healing can be achieved by combining them with psychotherapy.
What Are Neurotransmitters?
Neurotransmitters are messenger molecules that transmit signals between neurons. The brain’s 100 billion neurons rely on these chemicals to communicate efficiently, using electrical impulses and neurotransmitters to relay messages. Produced in the brain, these molecules bind to receptors in the synapses to ensure proper signal transmission. Despite their microscopic size, neurotransmitters play a powerful role in regulating mood, motivation, energy, sleep, and memory. Without them, thoughts, emotions, and movements would not function properly. Imbalances in these brain chemicals are often targeted through anxiety medication in Dubai and modern options like atypical antidepressants. In treatment-resistant cases, innovative solutions such as ketamine therapy in Dubai are gaining popularity for their fast-acting relief of depression and anxiety symptoms.
The Serotonin Hypothesis
The serotonin hypothesis dates back to 1969. Two scientists from Leningrad (now St. Petersburg) reported in depressed patients lower levels of a serotonin breakdown product in the brain fluid. Following this conclusion, they suggested that depression may stem from a serotonin deficiency.
The serotonin model became popular in medical textbooks and still exists in the popular opinion. However, later studies have failed to convincingly prove a serotonin deficit in depression. Depression is a complex condition; therefore, the idea that an imbalance of a single neurotransmitter could be the only root cause is outdated. The development of new antidepressants with no influence on the serotonin receptor proved this hypothesis wrong.
How Do Antidepressants Work?
Antidepressants influence the brain’s metabolism through neurotransmitters such as serotonin, norepinephrine, dopamine, and glutamate. Most antidepressants work by increasing the concentration of neurotransmitters in the so-called synaptic space. This happens by preventing the reuptake of neurotransmitters into “transmitter cells” (presynaptic neurons) after they have been released. This is also known as “no re-entry.” The increased concentration of the neurotransmitters exerts a stronger effect on the “receiving cell” (the post-synaptic neuron).
SSRIs Course of Action
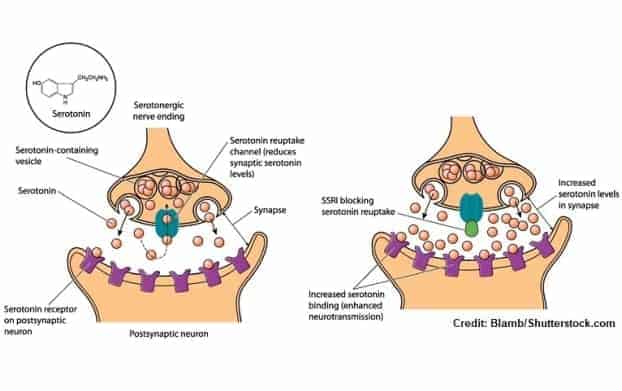
SSRIs (Selective Serotonin Reuptake Inhibitors) can be used as a model for antidepressants mechanism of action. The nerve cell, called neuron, consists of a body and the axon. The latter can be compared to an electrical wire. There are several neurons between the source of impulse and its receiver, which means that the electric impulse must “jump” from one neuron to the other. The transport of the information along the axon happens “electrically” through voltage changes on the cell wall. The information travels as an electrical wave to the end of the axon. However, the axons are not connected directly. There is the mentioned synapse, a gap between the corresponding neurons. The impulse must be past to the next neuron chemically through the neurotransmitters, in case of SSRIs trough serotonin.
The electric impulse arriving in the first neuron stimulates the release of serotonin in the synaptic space, which stimulates the second neuron. Afterwards serotonin is immediately taken back to the synapse of the first neuron. Premature or excessive reuptake, i.e., taking back the neurotransmitter into the neuron, lowers its concentration. The lower serotonin concentration slows the speed of the impulse traveling through the neural pathways. SSRIs block the excessive reuptake, leading to an increase in serotonin concentration in the synaptic space, and by doing so, they speed up the flow of the information in the brain.
SSRI vs. SNRI. The Difference
Serotonin plays a crucial role in regulating mood. When serotonin levels are too low, a person may experience depression, anxiety, suicidal thoughts, or obsessive-compulsive behaviours.
Norepinephrine is involved in the body’s fight-or-flight response. When a person feels threatened, norepinephrine naturally increases. In everyday life, norepinephrine also contributes to sleep, attention, memory, and mood regulation. People with low levels of norepinephrine may have trouble concentrating or experience depression.

Both SSRIs (Selective Serotonin Reuptake Inhibitors) and SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) increase serotonin concentration in brain areas associated with depression. Additionally, SNRIs also increase norepinephrine concentration in such areas. Higher norepinephrine concentration improves mood but also the energy level and concentration. There is no conclusive evidence that one of this group is consistently superior to the other. In clinical practice, the psychiatrist may need to try different SSRIs or SNRIs to find the most effective antidepressant and the most effective dosage while avoiding the side effects.
Tricyclic Antidepressants
The tricyclics are the oldest group among antidepressants. Such substances as imipramine, nortriptyline, amitriptyline, doxepin, trimipramine, and desipramine are effective, but they have more side effects than SSRIs and SNRIs. Tricyclics can be used for the treatment of depressions resistant to treatment with other groups of antidepressants.
Monoamine Oxidase Inhibitors (MAO)
Monoamine Oxidase Inhibitors (MAOIs) like tranylcypromine, phenelzine, and isocarboxazid, despite their strong anti-depressive effect, can be prescribed when other antidepressants don’t work. MAO inhibitors block an enzyme dismantling neurotransmitters such as serotonin, norepinephrine, and dopamine, increasing their concentration in the synaptic gap.
There are two groups of MAO inhibitors: irreversible and reversible. Irreversible MAOIs have a longer-lasting effect and interact with food containing tyramine, such as cheese, red wine, or chocolate. Patients treated with irreversible MAOI have to follow a strict low-tyramine diet. Reversible MAO inhibitors do not require such a diet.
Selegiline is a newer irreversible selective inhibitor of monoamine oxidase type B (MAO-B) that is applied as a patch and has fewer side effects. MAO-B is breaking down dopamine, which plays a crucial function for such cognitive functions as memorizing and concentration. MAO-B is effective in treating conditions with reduced dopaminergic neurotransmission, including Parkinson’s disease.
MAO inhibitors might create severe side effects if combined with other antidepressants or alcohol. They can rapidly increase the serotonin concentration in the synaptic space, causing life-threatening, so-called serotonin syndrome. In case the medication should be switched from irreversible MAO inhibitors to other antidepressants, a gap of three weeks should be maintained.
The less severe side effects of MAO inhibitors can be restlessness, insomnia, dry mouth, and digestive issues. In patients treated with MAO inhibitors, regular blood and liver function controls are necessary.
Atypical Antidepressants
Such newly developed antidepressants like Bupropion, Mirtazapine, Agomelatine, Nefazodone, Trazodone, and Vortioxetine don’t belong to any of the above-mentioned categories. They have different courses of action and can be used alone or in combination with other antidepressants. Scientists assume that they are the predecessors of new groups of antidepressants that are already in clinical trials or that can be developed in the near future.
Ketamine
Ketamine has an immediate, short-acting stimulating effect, and it’s not a proper antidepressant. It’s used in anesthesia, inducing sedation, pain, and dissociation (trancelike state). Ketamine on the molecular level has antagonistic properties on glutamate receptors and acts on serotonin and dopamine systems. Ketamine is also influencing the neuroplasticity of the brain increasing the number of synapses in brain areas related to depression.
At the end of 2019, the drug Esketamine has been approved by the FDA as a nasal spray for therapy-resistant depression. The biggest disadvantage of ketamine therapy is its short efficacy. After ketamine treatment, most patients experience a depressive relapse after around one week.
The hype about ketamine therapy is related to its immediate effect. The conventional antidepressants need weeks to take effect, so the rapid response of ketamine therapy is tempting. However, ketamine is associated with promises that the substance cannot keep because of the substantial risk of relapse.
The therapy with ketamine is intended primarily for inpatient treatment in psychiatric centers. Ketamine can be used only for individuals who have already undergone at least two sufficiently long therapy attempts with approved antidepressants in sufficient dosages.
Choosing Right Medication
The treatment of severe depression or depression with anxiety requires a combination of two, sometimes three, different substances. In people with severe anxiety and/or suicidal ideations, the administration of a sedating medication, especially at the beginning of the treatment, prevents the risk of suicide or overboarding anxiety. By choosing the right antidepressant and titrating its dosage, the side effects can be avoided.
Optimizing Treatment with Antidepressants
The initial step typically involves switching to a different antidepressant instead of combining two medications, as the evidence does not favor one strategy over the other. However, if combinations are considered, research suggests that combining SSRIs or SNRIs with Mirtazapine or Bupropion may be effective.
Changing the Antidepressant
When initial treatment optimization fails, switching to a different antidepressant is a viable option. However, selecting the new antidepressant should be based on factors such as the patient’s response history and potential side effects.
Combining Two Antidepressants
The combination of two antidepressants is another approach to consider in cases of treatment-resistant depression. Combining SSRIs or SNRIs with Mirtazapine or Bupropion has shown promise. However, the choice of combination should be made carefully, considering potential interactions and side effects.
Augmentation Therapy
This method involves adding a substance that doesn’t have acute antidepressant effects but enhances the efficacy of an antidepressant. This strategy may be preferred over switching antidepressants in cases of partial remission. Augmentation options include Lithium and atypical antipsychotics like Quetiapin, Aripiprazol, and Olanzapin, which are added to the existing antidepressant regimen.
Augmentation with Mood Stabilizers
As the name suggests, this medication possesses a mood-stabilizing effect, reducing the mood swings. They could be added to the treatment with antidepressants to enhance their effectiveness. Mood stabilizers can also be used in the phase prophylaxis, protecting the patients, especially those with recurrent depressive episodes, from relapses. The most effective mood stabilizers with such an effect are Lamotrigine and Lithium.
Lithium Augmentation
Lithium augmentation has been supported by prospective studies in older patients, showing significant benefits compared to a placebo. For older patients, a target serum level of 0.4 mmol/l may be sufficient, and if there’s no response within four weeks, a change in strategy is recommended. Successful augmentation should continue for at least a year. Recent research also suggests potential pro-cognitive and anti-dementia effects of Lithium.
Augmentation with Lamotrigine
Lamotrigine is frequently used and effective in the treatment of bipolar disorder, especially as a prophylaxis. However, lamotrigine also showed its efficacy as an augmentation agent in the treatment of refractory unipolar major depressive disorder. Studies revealed that lamotrigine was most effective in patients depressed for shorter periods of time who had failed fewer previous treatments with antidepressants. Lamotrigine seems to increase response in patients with comorbid anxiety disorders or chronic pain syndromes.
Augmentation with Atypical Antipsychotics
Atypical antipsychotics, particularly Aripiprazole and Quetiapine, can be used as augmentation strategies in cases of treatment-resistant depression. However, by their use, anticholinergic effects should be considered, as they can worsen cognitive function. Antipsychotics can be combined with antidepressants, especially in cases of severe depression with psychotic features or in cases of depression with OCD symptoms.
Augmentation with Stimulants
Stimulants, such as Methylphenidate, have been mentioned as augmentation strategies in treatment guidelines. However, the evidence for their use is inconsistent.
Adjuvant Medications
Antidepressants need several weeks to show positive effects. At the beginning of the treatment, they can even worsen the symptoms, triggering more anxiety or sleep deprivation. Therefore, in the initial treatment phase, a quick-acting medication with a calming and sleep-regulating effect is necessary.
The most frequently used adjuvant medications are benzodiazepines. These drugs serve primarily as hypnotics (sleep-inducing medication) and anxiolytics (anti-anxiety medication) in cases of severe insomnia or agitation. They are useful in the first days of treatment with antidepressants, especially in patients with severe anxiety, sleeplessness, or suicidal thoughts. Because benzodiazepines show an immediate calming effect, they help to “bridge” the gap until the antidepressant develops such an effect on its own.
FAQs about Antidepressants and Their Actions
In this section, we listed the common questions asked by our patients.
CHMC is a German Psychiatric Clinic in Dubai. We are specialized in the treatment of distinct psychiatric disorders. Usually, an answer to an anonymous question will never be fully satisfactory. A psychiatric diagnosis and the following therapy are effects of the initial in-depth assessment and the following good personal contact with the patient.
I don’t want to use antidepressants…
Question:
I have been diagnosed with depression but I’m scared to take antidepressants. Do you think I can overcome the depression with counselling? Where can I get help in Dubai?
Answer:
We understand your worries. The Internet is full of negative reviews about antidepressants. One of the frequently heard complaints is that they have several side effects; the second is that you can get addicted to them. However, the antidepressants are the cornerstones of the psychiatric treatment of depression and anxiety disorders. The biggest advantage of them is that they are not addictive. In the hands of an experienced psychiatrist, the side effects can be fully avoided.
We are not able to answer your question about whether the counselling would be enough for sufficient treatment of your depression. If the symptoms are very mild, this could be the case. In moderate and severe depression impacting massively your life, it’s unlikely that you will recover in a foreseeable time from depression. In general, the antidepressants are fast, and they shorten the period of treatment for depression. Nevertheless, you would need in parallel the counselling, as the antidepressants are not a remedy for your life problems. They suppress the symptoms, giving you time and a “clear head” to implement the changes.
I’m moving to Dubai. Currently I’m taking an antidepressant. Can I get it in Dubai?
Question:
I’m living in the UK, and I’m taking an antidepressant. Are the antidepressants legal in Dubai? Where can I get them?
Answer:
Antidepressants are legal in Dubai. In order to continue the treatment, you should contact a psychiatrist in Dubai to continue your treatment.
I work in the IT sector in Dubai. Because of my growing fatigue, I’ve been told to take antidepressants…
Question:
I worked for 6 years in an IT company in Dubai, getting increasingly more stressed out and tired. The symptoms appeared gradually around 1.5 years ago. I do psychotherapy, but it helped only a little. My psychologist recommended visiting a psychiatrist and taking antidepressants. However, I’m scared to become a zombie. How do the antidepressants work? Should I have concerns about using them?
Answer:
The common misconception about antidepressants is that they create an artificial state of mind and feelings. Properly applied antidepressants can lift mood and energy to a normal level and regulate sleep. With more serious depression counselling/psychotherapy wouldn’t be possible without controlling the symptoms of depression with medication. The antidepressants create a kind of protective umbrella, allowing the patient to keep the day-to-day routine, giving him time to implement the changes ideally supported by psychotherapy. After gradual removal of the antidepressants the patient shouldn’t feel any difference compared to his feeling under the pharmacotherapy. An antidepressant used by someone who is not depressed will not have any effect.
Are pills the best way to get out of depression?
Medications can suppress the symptoms of depression and keep you functional, but they will not solve your problems. If you rely only on tablets without getting insight into your problem, the symptoms will appear again even by keeping the same dosage of medication. It’s not only our personal experience that in cases of moderate and severe depression, the combination of medication and counselling is much more effective than one of the methods applied alone.
Are antidepressants necessary for every depression?
For mild depression, comprehensive treatment strategies such as the use of psychotherapy, sports exercises, and meditation should be tried first. Patients with moderate and severe depression require a combination of antidepressants and psychotherapy. Those patients also benefit from integrative treatment methods such as meditation, art and music therapy, or acupuncture.
Do antidepressants create side effects?
Prescribed by an experienced psychiatrist, using the proper antidepressant and titrating slowly the dosage, the side effects can be avoided. Starting with a high dosage or the wrong antidepressants, the symptoms can be aggravated. We are aware of the worries and prejudices about the use of psychiatric medication. Our aim is to remove the symptoms without creating side effects.
Do people feel numb taking antidepressants?
This is a very frequent misconception related to the effect of antidepressants. A proper antidepressant in a proper dosage shouldn’t create any feeling of numbness.
Are antidepressants addictive?
Antidepressants are not addictive. The effect of an antidepressant appears gradually over weeks. In consequence, there is no causal connection between the intake and the effect.
I gained weight on Escitalopram…
Question:
I’ve been living in Dubai for 6 years; for 2 years I’ve been taking Escitalopram, but I gained weight. Should I stop it?
Answer:
Indeed. Some antidepressants, especially SSRIs, to which belong Escitalopram, can cause weight gain as a side effect. Stopping the medication on your own, especially stopping it abruptly, is not a good idea. You will get unpleasant discontinuation symptoms such as diarrhea, headache, or nausea. However, if you reduce the medication gradually, you will experience such discontinuation symptoms. The other problem is that a few weeks later you can dip again into depression. Any changes of medication should happen under the supervision of your psychiatrist.


