
At CHMC Dubai, we provide expert ADHD diagnosis and treatment led by Dr. Gregor Kowal, a German Board-Certified Consultant Psychiatrist and Psychotherapist.
Attention Deficit Hyperactivity Disorder (ADHD) is a developmental disorder. It is characterized by symptoms of inattentiveness, over-activity, impulsivity, or combination of both.
Peaple with ADHD have difficulties with organization, maintaining concentration, emotional regulation, and impulsivity. These neurocognitive deficits often interfere with people’s daily routine, work performance, and relationships.
Initially ADHD was understood as a childhood disorder. Over time psychiatrists noticed that the symptoms also persist in adults.
ADHD in adulthood impairs an individual’s social and professional performance just as significantly as in childhood. Therefore, it’s highly important to acknowledge that ADHD is a treatable condition and highlights the importance of early diagnosis and therapy.
For ADHD Treatment in Dubai Make an Appointment with Our Leading Psychiatrist Dr.Kowal
Call CHMCCore Symptoms of ADHD
The following three core symptoms are characteristic of ADHD:
Hyperactivity:
Marked restlessness that shows through constant fidgeting, shifting in the chair, or climbing. For example, repeatedly tapping the foot, drumming fingers, or avoiding situations that require sitting still for a longer time.
Attention Deficit (Impaired Concentration):
Difficulty focusing attention, short attention span, and being easily distracted. This may appear as forgetfulness, careless mistakes, trouble following instructions, or starting new tasks before finishing the previous ones.
Impulsivity:
Acting or speaking without considering the consequences. This often shows as interrupting others, making hasty decisions, being more prone to accidents, ignoring rules, or sudden outbursts of anger.
However, the intensity of these symptoms can vary, and not all of them need to be present at the same time.
As individuals grow older, the ADHD symptoms often become less pronounced compared to the earlier stages of childhood and adolescence.
Additional Symptoms in ADHD
The core symptoms of ADHD – inattention, hyperactivity, and impulsivity – rarely occur alone. Often, affected children with ADHD have other problems that can change as they age. Unpleasant experiences and negative interactions occur more frequently between parents, teachers and the child or adolescent. Most commonly, children and adolescents with ADHD also exhibit oppositional and aggressive behaviours.
Conflicts with parents, teachers and peers
A variety of children and adolescents with ADHD are often rejected by their peers. This can happen because they constantly disrupt play due to their ADHD symptoms or because their aggressive behaviours are perceived as bullying.
Due to the frequently socially inappropriate behaviours of children and adolescents with ADHD, parents often have increased conflicts with their child, and the relationships between parents and child are often highly strained.
Oppositional and aggressive behaviour
Most commonly, children and adolescents with ADHD also exhibit oppositional and aggressive behaviours. These behaviours include not following important rules in the family, kindergarten, and school. Additionally, they do not respond to instructions from adults, often have outbursts of anger, and engage in frequent conflicts with siblings and other children.
In adolescence, it can occur that individuals with ADHD disregard important social rules. This can lead to various behaviours: some lie to gain advantages, some steal within or outside the family, or they skip school and stay out later at night than allowed. As a result of theft or property damage, individuals with ADHD often eventually come into conflict with the law.
Tics
Motor tics are sudden, involuntary movements such as eye blinking, nose twitching, or jerking of the head. Vocal tics are involuntary vocalizations, such as throat clearing, or even words and phrases that are suddenly spoken out. Such tics occur more frequently in children with ADHD, often starting in childhood and persisting into adolescence and adulthood.
Course of ADHD in Adulhood
In adults, ADHD is usually less obvious than in hyperactive children or teenagers. Adults with ADHD mainly struggle to organize their daily life or work, and stay focused on tasks for longer periods.
They can also be very impulsive. For example, adults with ADHD may talk a lot and frequently interrupt others. Some lose their temper quickly, end relationships prematurely, switch jobs suddenly, or quit before securing a new position. Difficulties can also arise in traffic, for instance through reckless driving.
Many adults with ADHD find it hard to keep their emotions balanced. They are easily irritated and have a low tolerance for frustration.
Many untreated ADHD patients have histories of negative academic and professional performance, often falsely attributed to their low intelligence. However, scientific data has proven that people with ADHD are often smarter than average.
Therfore, it’is important that an ADHD diagnosis is made carefully to avoid unnecessary or incorrect treatment.
ADHD Diagnosis at CHMC Dubai
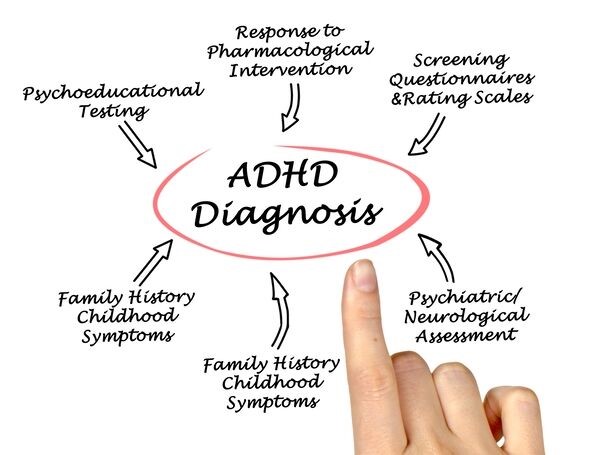
ADHD is defined as a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with daily functioning. It is often hard to draw the line between normal and hyperactive behavior and to identify a clinically significant level requiring intervention.
Because other mental health disorders can cause symptoms similar to ADHD, it’s easy to misdiagnose such conditions. Therefore, it’s important to secure the diagnosis through a reliable and thorough assessment.
In order to make a precise ADHD diagnosis, we cooperate closely with the patient himself as well as his parents, caregivers or fiends. At our psychiatric clinic in Dubai we make ADHD diagnosis based on the DSM-5 guidelines.
ADHD diagnosis in adults has the following five or more symptoms of inattention and/or 5 or more symptoms of hyperactivity/impulsivity. They must have persisted for more than 6 months.
ADHD Criteria According to DSM-5
To be diagnosed with ADHD, the following conditions must be met:
Early Onset: Some symptoms of inattention or hyperactivity-impulsivity must have been present before the age of 12.
Across Different Situations: Symptoms need to show up in at least two settings – for example, at home and school, at work and with friends, or in other social activities.
Impact on Daily Life: There must be clear evidence that the symptoms interfere with or lower the quality of social life, school performance, or work functioning.
Not Better Explained by Another Disorder: The symptoms cannot be explained solely by another mental health condition, such as depression, anxiety, or a personality disorder.
In short, ADHD is diagnosed when symptoms begin in childhood, appear in different areas of life, and cause significant problems in daily functioning – while ruling out other possible explanations.
Diagnostic Assessment for ADHD at CHMC Dubai
Adults generally show fewer motor restlessness symptoms due to their ability to hide or control them. Even so, adults may remain overactive, inattentive, impulsive, poorly organized, and emotionally unstable.
Diagnosing ADHD in adults is a detailed process that takes time and care. It cannot be confirmed with a single test or questionnaire. Consulting a psychiatrist at CHMC ensures a complete and reliable diagnosis combining different approaches — medical, psychiatric and psychological.
A specialist can:
- Confirm whether symptoms truly meet ADHD criteria
- Exclude physical or psychiatric disorders that look similar
- Provide ADHD medication if needed
- Offer psychotherapy to enhance the focus and emotional regulation
ADHD is manageable when treated properly. Our psychiatrist uses a combination of medication, psychotherapy and lifestyle strategies to help patients regain focus, motivation, and balance.
Step 1: Clinical Interview
The first and most important step in diagnosisng ADHD is a comprehensive interview. It provides important informations into an individual’s history, symptoms, and overall functioning. This helps comprehend several cognitive dimensions, such as attention, memory, and executive functioning.
The other important scope of clinical interview is ruling out other psychiatric disorders which might affect the concentration such as depression, anxiety, or bipolar disorder.
It can be helpful if a partner, parent, or friend joins the evaluation to share observations from another perspective. They can describe situations where the person’s attention or behaviour seemed different, giving also insights into patient’s childhood.
Step 2: ADHD Questionnaires
After the interview, standardized ADHD questionnaires are used to measure the symptoms more precisely. These forms can be filled out by the patient and, with consent, by close people such as a partner, colleague, or family member. This helps show how symptoms appear in different environments — at home, work, or social settings.
Step 3: Ruling Out Other Causes
A responsible psychiatrist in Dubai always checks for other possible explanations. Several medical or psychological conditions — such as thyroid disorders, depression, anxiety, or sleep problems — can cause similar symptoms. Therefore, a physical check-up and blood tests are often part of the process.
Step 4: Psychological and Behavioral Tests
Sometimes, cognitive or psychological tests are added to understand how attention, memory, and planning skills work. Adults with ADHD often do not show the same physical restlessness seen in children, but subtle signs may appear — tapping fingers, fidgeting, or a sense of internal tension.
CHMC offers psychometric tests It as an evidence-based, and practical tool spotting the ADHD symptoms.
Treatmant Options for ADHD at CHMC Dubai
A diagnosis alone does not automatically mean that treatment for ADHD is necessary. The decision depends on the severity of symptoms and the degree of psychological, social, or occupational impairment.
When treatment is indicated, it may include medication, psychotherapy, and psychoeducation.The entire process of ADHD treatment usually involves combination of medications, psychotherapy, behaviour modifications and lifestyle changes. Multiple studies proved that the best ADHD treatment results are achieved using combination of medication and psychotherapy.
ADHD Treatment in Dubai with Medication
Treatment with medication is the main pillars for the ADHD treatment.
When doses are adjusted carefully and monitored professionally, medications help reduce inattention, impulsivity, and emotional instability. They support better performance at work, more stable relationships, and improved overall quality of life.
Untreated ADHD has a negative impact on many areas of life; it carries a high risk of additional psychiatric disorders and contributes to significant societal costs.
Therefore, beginning the treatment of ADHD with medication early is highly relevant.
Medication called “stimulants” is the first-line pharmacological treatment for ADHD. In the UAE just like in other countries stimulants have the status of “narcotic medication.” Psychiatrists prescribe this medication under conditions of strict documentation and close patient monitoring.
How Medications for Treatment of ADHD Work
ADHD is linked to an imbalance of neurotransmitters, especially dopamine and noradrenaline, in the prefrontal cortex, a brain region responsible for focus, attention, and impulse control.
Stimulant medications counteract this imbalance by slowing the reuptake of dopamine and noradrenaline. This allows the neurotransmitters to remain active longer, increasing alertness, concentration, and mental performance.
It may seem unusual to treat hyperactivity with stimulating medication. However, this medication has actually a calming effect on ADHD patients. Therefore, the risk of dependency in accurately diagnosed patients is negligible. Nevertheless, in order to reduce the risk of habit-forming behaviour the medication of choice are slow-release stimulants, like Concerta containing Methylphenidate or Vyvans containing Lisamphetamine.
A careful titration of the medication used for ADHD treatment and regular laboratory and ECG controls help to exclude potential side effects. If these criteria are met, the benefits of treatment far outweigh the possible risks.
Atomoxetine works differently. It selectively blocks the reuptake of noradrenaline, which helps improve attention and reduce impulsive behaviour. Guanfacine also affects noradrenaline signaling, although its exact mechanism in ADHD is not fully understood.
Medications Available in Dubai for Treatment of ADHD
For the treatment of ADHD with medication, several groups of drugs are used. Stimulants such as methylphenidate (MPH) and amphetamine are considered first-line treatment.
Atomoxetine (ATX), a noradrenaline reuptake inhibitor, also plays an important role and is not classified as a stimulant.
Guanfacine and dexamphetamine have not been sufficiently studied in adults. Due to limited evidence, they are not approved in Dubai.
A dopaminerg antidepressant, such as Bupropion, may also be used when other treatments are not suitable.
The main active substances used today for treatment of ADHD in Dubai include atomoxetine, methylphenidate, and lisdexamfetamine.
Treatment usually begins with a low dose, which is gradually increased until symptoms improve.
ADHD Treatment with Methylphenidate
Methylphenidate is a psychostimulant used to treat attention-deficit/hyperactivity disorder (ADHD) and narcolepsy. It was first introduced to the market in 1954 under the brand name Ritalin.
Methylphenidate is available in several formulations that differ mainly in the way the active substance is released. These pharmaceutical differences determine whether the medication takes effect immediately or is released gradually over a longer period, which influences the duration of action.
The choice of preparation depends on the patient’s individual needs. Immediate-release formulations allow flexible dosing but require more frequent intake, while extended-release formulations provide a steadier and longer effect, which can be especially useful in daily routines or school settings.
Immediate-Release Formulations
This form of methylphenidate is released quickly after ingestion and reaches its effective blood level within 30 to 60 minutes. The effect usually lasts three to four hours, which often makes multiple daily doses necessary.
In Dubai, the immediate-release version is available under the brand name Ritalin. These tablets are often taken in the morning and afternoon to maintain consistent symptom control throughout the day, though they need to be taken at regular intervals.
Extended-Release Formulations
To achieve a longer-lasting effect and reduce the number of daily doses, extended-release methylphenidate was developed. These formulations release the active substance continuously over an extended period.
This is achieved through specialized pharmaceutical technology that binds the medication in different layers or reservoirs. As a result, methylphenidate is released in several phases: an initial immediate release followed by a slow, continuous release over several hours. In Dubai, the extended-release form of methylphenidate is available under the brand name Concerta.
Treatment for ADHD with Atomoxetine
Atomoxetine, marketed in Dubai under the brand name Strattera, is a selective norepinephrine reuptake inhibitor. It is the first ADHD medication classified as a non-stimulant and therefore not subject to narcotics regulations. Atomoxetine is approved for adults when ADHD symptoms were present during childhood. It is often chosen when stimulants are not tolerated or not advisable. Atomoxetine is generally well tolerated and has no potential for misuse or dependence.
Clinical studies have shown that atomoxetine significantly reduces the core symptoms of ADHD: inattention, hyperactivity, and impulsivity. Improvements have also been observed in psychosocial areas such as self-esteem and family interactions.
Atomoxetine’s effectiveness is comparable to that of methylphenidate, and the response rate is similarly around 80 percent. Although many patients begin to notice an effect after about one week, it generally takes four to six weeks to reach full therapeutic benefit.
A major advantage of atomoxetine is that a single morning dose provides continuous symptom control until the next day. Atomoxetine is often considered when patients continue to experience symptoms at critical times—such as early in the morning—despite treatment with methylphenidate, or when methylphenidate is poorly tolerated.
Lisdexamfetamine Tretament for ADHD
Lisdexamfetamine is used in the treatment of attention-deficit/hyperactivity disorder (ADHD). It belongs to the group of synthetic amphetamines and is regulated under narcotics legislation.
Lisdexamfetamine itself is pharmacologically inactive. After oral intake, it is rapidly absorbed in the gastrointestinal tract and converted primarily by red blood cells into dexamfetamine, the active metabolite. The plasma half-life of lisdexamfetamine is generally less than one hour. Because the half-life of dexamfetamine is around 11 hours, a single dose of lisdexamfetamine provides symptom control throughout the day. In Dubai, lisdexamfetamine is marketed under the brand name Vyvanse.
The substance increases the availability of the neurotransmitters norepinephrine and dopamine in the synaptic cleft by inhibiting their reuptake. The exact way in which this process leads to improvement in ADHD symptoms is not yet fully understood.
Possible Side Effects of ADHD Medication
Stimulant medications such as methylphenidate and lisdexamfetamine may cause gastrointestinal discomfort, dizziness, high blood pressure, heart palpitations, headaches, increased restlessness, sometimes accompanied by sleep disturbances. Because of frequent sleep disturbances, these medications should not be taken late in the day.
Psychotherapy Treatment for ADHD at CHMC Dubai
While medication is often the first-line treatment for ADHD, psychotherapy plays als an important role. Therapy helps patients develop strategies to manage symptoms, improve daily functioning, and strengthen relationships. At CHMC Dubai, we combine proven psychological methods with individualized care.
Cognitive Behavioral Therapy (CBT) in Treatment for ADHD
CBT is one of the most effective psychotherapy technics for ADHD. It focuses on identifying unhelpful thought patterns and replacing them with healthier ones. For patients with ADHD, CBT helps in breaking down overwhelming tasks, reducing procrastination, and managing frustration. Techniques such as using reminders, setting realistic goals, and practicing self-monitoring are often introduced during sessions.
Behavioral Therapy for ADHD
Behavioural therapy includes practical help by organizing tasks or dealing with emotionally challenging events working through positive reinforcement for desired behaviours. It helps the patient and his family to understand and to gain control of the stressful feelings related to ADHD. Parents are often involved in the process, learning how to give clear instructions, set consistent rules, and reward progress. Over time, children gain more control over their impulses and improve their interactions at home and school.
ADHD Mindfulness-Based Therapy
Many individuals with ADHD struggle with restlessness and racing thoughts. Mindfulness-based interventions teach them how to focus attention on the present moment, reduce emotional reactivity, and increase self-awareness. Studies show that mindfulness practices can improve attention span and decrease impulsivity in both children and adults.
Skills Training for Individuals with ADHD
ADHD coaching is a practical form of therapy designed to improve organization and time management. Patients learn strategies to structure their daily routines, prioritize tasks, and build sustainable habits. Skills training can be especially useful for adults balancing work and family responsibilities.
Family and Couples Therapy for ADHD
Since ADHD often affects family life, therapy may involve parents, partners, or spouses. Family therapy helps reduce conflict, improves communication, and fosters better understanding of ADHD-related behaviors. In couples therapy, the focus is on resolving misunderstandings and building supportive strategies to manage challenges together.
Therapy Based on ADHD’s Severity
Specifying the severity of ADHD is not just a diagnostic formality. It helps guide treatment planning, determine the urgency of intervention, and set realistic goals. A patient with mild ADHD may benefit primarily from behavioral strategies and skills training, while someone with severe ADHD may need structured therapy, medication, and ongoing support. Understanding the severity also allows families, teachers, and employers to adjust expectations and provide appropriate accommodations.
Severity Specification of ADHD
Mild – few, if any, symptoms in excess of those required to make the diagnosis are present. The symptoms result in no more than minor impairments in social or occupational functioning.
Moderate – symptoms or functional impairment between ‘mild’ and ‘severe’ are present.
Severe – many symptoms in excess of those required to make the diagnosis, or several symptoms that are particularly severe.
Diagnostic Problems in ADHD
In adults ADHD the signs and symptoms may differ from those during childhood due to the adaptive processes and avoidance mechanisms learned during the process of socialization. Many adults with ADHD are even not aware that they have the condition. An in-depth clinical interview of such individuals will uncover history of failure at school, problems at work, failed relationships, or multiple traffic accidents.
Misdiagnosing ADHD with Other Conditions
Another barrier to the diagnosis of ADHD in adulthood is the blurring of the boundaries between ADHD and other psychiatric disorders. Mood and anxiety disorders are often misdiagnosed as ADHD.
Adults-ADHD and Psychiatric Co-Morbidities
ADHD is also frequently linked to other psychiatric conditions, especially substance misuse, mood disorders, anxiety, and personality disorders. That’s why, a thorough clinical examination is required to confirm the diagnosis of ADHD, differentiating it from other psychiatric disorders. This helps to exclude overlapping comorbidities, such as depression or anxiety disorders, which also impairs the performance of ADHD individuals.
Prevalence of ADHD
ADHD is a common mental disorder. The exact prevalence (Proportion of affected individuals in 100 people of a particular population) numbers vary depending on which criteria (according to ICD-10 or DSM-5) are used for diagnosis and how the diagnosis is obtained.
Globally, an average prevalence rate of around 4% to 6% is assumed for children and adolescents, using the less strict diagnostic criteria according to the American classification system DSM-5. When the very strict criteria of ICD-10 are used, the rate is estimated to be 1 to 3%.
In all studies, gender-specific differences in the prevalence of ADHD can be observed, with boys being significantly more affected than girls.
Despite the evidence that ADHD symptoms continue lifelong, until today very few adults receive adequate treatment. One study conducted in the United States estimated that only 10% of adults suffering from ADHD received treatment. This means that up to nine million adult Americans remain untreated.
ADHD Treatment in Dubai. Summary
For many years ADHD was mistakenly regarded as a disorder that only affects children and adolescents. However, research has shown that symptoms often continue into adulthood.
ADHD is of major social and economic importance. It can cause significant psychological and social impairment. Proper treatment of ADHD can reduce symptoms and improve functioning.
For many adults, medication for treatment of ADHD plays an essential role in daily functioning. When doses are adjusted carefully and monitored professionally, medications help reduce inattention, impulsivity, and emotional instability. They support better performance at work, more stable relationships, and improved overall quality of life.
Beginning the treatment of ADHD with medication early is highly relevant. Untreated ADHD has a negative impact on many areas of life; it carries a high risk of additional psychiatric disorders and contributes to significant societal costs.
The psychotherpay and skills trainig plays a complementary role in treatment for ADHD.
FAQ about ADHD
The first step in the treatment of ADHD is contacting a psychiatrist or psychologist to secure the diagnosis. In the majority of the cases the symptoms of ADHD can be fully controlled allowing the individual normal work and social performance. Our German Clinic for Psychiatry and Psychology in Dubai is specialized in treatment for distinct psychiatric disorders, among them therapy for Attention Deficit Hyperactivity Disorder (ADHD).
In the below text we answer the most common question about diagnosis and treatment of ADHD.
What is ADHD?
ADHD is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with daily functioning and development. ADHD is an in-born condition and can’t be outgrown.
The treatment of ADHD depends on its severity and its impact on your social and professional life.
What kind of problems are associated with ADHD?
Look for these common problems:
- Inconsistent job performance,
- frequent job changes
- History of academic or career underachievement
- Difficulty managing daily tasks, bills, and chores.
- Relationship strains due to unfinished tasks.
- Forgetfulness, frustration, and intense worry about unmet goals
- Carelessness, neglecting detail.
- Starting tasks but not finishing.
- Poor organisational skills.
- Lack of focus, prioritisation.
- Frequent item loss.
- Restlessness, edginess.
- Impulsiveness, talking out of turn.
- Interruptions, blurting out.
- Mood swings, irritability, quick temper.
- Stress handling difficulty.
- Extreme impatience.
- Risk-taking, disregard for safety.
A professional can assess if these issues stem from ADHD or other causes. The life course of ADHD depends on several factors. While some individuals show symptoms early, others face challenges later in life. Bright individuals might compensate until high school.
Can adults have ADHD?
ADHD typically manifests in childhood; nonetheless, it can persist into adulthood. In the majority of cases, ADHD is diagnosed and treated in childhood; however, some adults may receive the diagnosis later in life. Moreover, the psychiatric diagnosis of adult ADHD was introduced in the late 90s. Consequently, if you weren’t diagnosed with ADHD as a child and you are in your forties, you didn’t have any chance to be diagnosed and treated during your adolescence and young adulthood.
Additionally, adult ADHD symptoms may differ from those in children due to physical and maturity differences, as well as variations in life circumstances. For instance, adults may experience intense restlessness that exhausts others instead of overt hyperactivity. As time passes, adults often develop coping mechanisms to mitigate their symptoms. Additionally, adults can exhibit any of the three subtypes of ADHD.
How does ADHD manifest in adults?
Adult ADHD is less apparent than in hyperactive children and adolescents. Adults with ADHD primarily struggle with organising their daily lives or work, maintaining focus on tasks for extended periods, or meeting deadlines.
However, they can also be very impulsive. For instance, adults with ADHD tend to be talkative and frequently interrupt others. Some may easily get into trouble, end relationships prematurely, switch jobs abruptly, or resign without having a new position lined up. Difficulties can also arise in traffic due to reckless driving.
Many adults with ADHD find it challenging to regulate their emotions. They are easily irritable and have a low frustration tolerance. When under stress, fulfilling their responsibilities becomes difficult. Adults with ADHD may also encounter difficulties in setting and achieving goals.
It’s highly advisable to seek professional advice when someone experiences symptoms of ADHD that significantly and persistently affect their quality of life. Therefore, it’s crucial to ensure a careful ADHD diagnosis to avoid unnecessary or incorrect treatments, keeping in mind that other psychiatric conditions can be misdiagnosed as ADHD.
I have been diagnosed with ADHD. Where I can get ADHD treatment in Dubai…
I just arrived in Dubai and I’m planning to live here for a couple of years. I’ve been diagnosed with ADHD in my home country.
Answer:
Our psychiatric clinic offers ADHD treatment in Dubai. In the first step we have to verify your diagnosis. The refill of the medication should be done in person in 3-4 weeks intervals.
How is ADHD recognized, and where can I be diagnosed in Dubai?
Diagnosis of ADHD involves a comprehensive evaluation by a qualified healthcare professional, which may include a review of symptoms, medical history, behavioural assessments, and input from parents, teachers, or caregivers. Our psychiatric clinic in Dubai provides the diagnostics for ADHD. You will find more information in our article about ADHD.
I’m taking Concerta. Can I get it in Dubai?
Concerta containing Methylphenidate is available in UAE. As a narcotic medication Methylphenidate can be prescribed only by a psychiatrist. To be prescribed with Concerta the clinic has to create a treatment file with meticoulus monitoring the dosage and the number of prescribed tablets.
I noticed reduced focus and procrastination…
I work in Dubai as an accountant. In the past 2 years, I noticed reduced focus and procrastination. I heard that those might be the symptoms of ADHD. How and where can I secure the diagnosis?
Answer:
Symptoms of ADHD include difficulty paying attention; moreover, there is excessive fidgeting or restlessness, impulsivity, forgetfulness, difficulty organizing tasks, and frequent interruptions during conversations or activities, along with procrastination.
ADHD can present in different shapes: ADHD Types and Behavioral Problems. However, if you didn’t notice such symptoms earlier (in your childhood), your inattentiveness might be caused by different psychiatric conditions, for instance depression, anxiety or a physical illness like hypothyreosis.
In our psychiatric clinic in Dubai we provide psychiatric and psychological assessment of ADHD.
At which age does ADHD typically emerge?
Symptoms of ADHD often become noticeable in childhood, typically before the age of 12. Nonetheless, some individuals may not receive a diagnosis until later in life when symptoms persist and interfere with daily life.
What causes ADHD?
While the precise cause of ADHD remains unclear, its development is likely influenced by a combination of genetic, environmental, and neurobiological factors. If a family member has ADHD, there is a 1 in 4 chance of inheriting the condition. You can find more information in our articles about causes of ADHD.
What are the treatment options for ADHD in Dubai?
Treatment for ADHD at CHMC in Dubai typically includes a combination of medication, behavioral therapy, and educational interventions. Behavioral therapy focuses on developing coping skills, organizational strategies, and behaviour management techniques.
What kind of medication for ADHD is accessible in Dubai?
In Dubai we have only two stimulants Methylphenidate as fast (Ritaline) ans slow-release (Concerta) tablets, long acting Lisamphetamine (Vyvans) and Atomoxetine (Stratera). They have different pharmacological course of action. For instance, while Methylphenidate and Lisamphetamine work immediately after the intake, Atomoxetine works similar to an antidepressants developing its full efficacy after few days to few weeks.
Can ADHD be outgrown?
While some individuals may experience a reduction in symptoms as they mature, ADHD is a life-long condition. Nevertheless, ADHD symptoms can be effectively managed with appropriate treatment and support.
ADHD can manifest differently while the individual grows older. Here our article about life course of ADHD.
How does ADHD affect daily life?
ADHD can impact various aspects of daily life, including academic and work performance, social relationships, self-esteem, and emotional well-being. With proper management and support, individuals with ADHD can learn to cope with their symptoms and lead fulfilling lives.
I’m living in Dubai, and I’m taking ADHD medication for 10 years. Is there any option to stop it without getting the ADHD symptoms?
Unfortunately, there is no cure for ADHD, but symptoms can be managed effectively with ongoing treatment and support. With the right combination of medication and psychotherapy, individuals with ADHD can learn to thrive and succeed in various areas of life. The Multimodal Treatment Study about ADHD shows that the most effective therapy for ADHD is the treatment with medication. The psychotherapy can improve your status a little, especially getting the same effect with lower dosage of medication.
If we look from different perspective ADHD is not a typical disorder. It’s a particular “brain wiring” making the individuals highly effective for dealing with particular tasks.
I have problems to maintain focus but I’m not hyperactive. What is the difference between ADHD and ADD?
The distinction between ADHD and ADD lies in their historical terminology and diagnostic criteria. Originally, ADD, or Attention Deficit Disorder, described individuals primarily struggling with attention-related issues without significant hyperactivity or impulsivity. However, with the DSM-5 revision in 2013, the term ADD was replaced by the ADHD-Inattentive subtype.
This update consolidated the diagnosis under ADHD, recognizing that inattentive symptoms could occur independently or alongside hyperactive/impulsive traits. Therefore, while ADHD encompasses both inattentive and hyperactive/impulsive presentations, the term ADD is no longer used in clinical diagnosis. As per the new terminology you might have ADHD-Inattentive subtype.
Where I can get ADHD assessment in Dubai?
Our psychiatric clinic offers ADHD assessment and treatment in Dubai. The first step would be to secure the diagnosis by using a psychometric test. Based on that we can differentiate 1. if you have ADHD 2. if so, then what is its presentation hyperactive or inattentive. Then we offer treatment plan for your ADHD.
What is the best medication to for ADHD. Where I can get it in Dubai?
Determining the best medication for ADHD varies from person to person, and it’s typically based on individual medical and psychological factors. Stimulant medications are commonly prescribed and have shown efficacy for many ADHD patients (70-80%). However, they may not be suitable for everyone, and some individuals may prefer alternative treatment options. Ultimately, we will work with you to find the most appropriate medication based on your specific needs and preferences. In Dubai we have only two stimulating medications such as Methylphenidate and Lisamphetamine; the other substance, Atomoxetine works slower showing the full effect after several weeks.
What other conditions are concurrent with ADHD?
Approximately two-thirds of individuals with ADHD also have at least one other coexisting condition.
The most prevalent mental health disorders that frequently accompany ADHD include anxiety disorders (including OCD), mood disorders (such as major depressive disorder, bipolar disorder), substance use disorders, personality disorders, disruptive behaviour disorders (including oppositional defiant disorder and conduct disorder), learning disorders, sleep disorders, and autism spectrum disorder. Additionally, tics and Tourette syndrome are commonly comorbid with ADHD.
I think I have ADHD. Where can I check in Dubai if I have ADHD?
Our psychiatric clinic in Dubai provides comprehensive diagnosis and treatment of ADHD. Our psychologists can assess if you have ADHD using psychometric testing. Once the diagnosis is secured we will develop for you a treatment plan.
How can you find out that I have ADHD?
ADHD is a malfunction of a certain brain area. It never appears “out of the blue”. The events of “zoning out”, lack of focus and hyperactivity can be traced back to your childhood. Therfore, the first step in diagnosing ADHD is to gather information about your history, especially school and work performance. Consecutivelly your diagnosis can be secured by a psychometric test.
ADHD. Whom to Ask for Support?
Adults with ADHD usually seek assistance from specialised medical professionals such as psychiatrists or psychologists. When young individuals with ADHD reach adulthood, it is advisable to start searching for an adult psychiatrist. However, in some cases, individuals who have turned 18 can continue receiving treatment from their child and adolescent psychiatrist until they reach the age of 21.
Who can diagnose ADHD in Dubai?
ADHD diagnosis in adults requires licenced mental health professionals or physicians: clinical psychologists, psychiatrists, neurologists, family doctors, or clinical social workers. Check their expertise in adult ADHD, as knowledge outweighs professional degrees. Reliable experts readily share their qualifications. At CHMC you will fina a team of experts specialized on diagnosis and treatment of ADHD.
What Helps to Deal with ADHD?
Many adults with ADHD face challenges primarily due to their inattention and impulsivity. However, some develop effective strategies to deal with it, for example by:
- Carefully planning the day and creating reminder lists to avoid forgetting things, while being mindful not to take on too much.
- Breaking tasks down into smaller steps to make it easier to accomplish them gradually.
- Placing reminders in important locations, such as the front door, refrigerator, or car, to aid memory.
- Recording important appointments and tasks in a notebook or mobile app.
- Establishing routines and consistently keeping essential items like keys or wallets in the same place.
Since the challenges of ADHD are highly individual, it is difficult to provide universally applicable advice. However, many individuals discover over time what can help them navigate daily life more effectively. Support from friends and family proves valuable in this process.
What is covered in the psychological assessment of ADHD?
Our comprehensive evaluation includes:
- In-depth clinical interview and diagnostic screening.
- Gathering reports from the patient and parents about symptoms and functioning.
- Self-report measures from the patient and parents.
- Analysis of all assessment results.
- Explanation of results to patients.
- Formulation of a diagnosis.
- Recommendations for treatment and referrals.
Can I expect support for ADHD from my company and friends?
Individuals with ADHD often question whether they should share their diagnosis with others. Close friends and family members may already be aware, but the situation can be different in the workplace. Deciding whether to inform colleagues or supervisors about one’s diagnosis is a challenging and personal consideration. Many people choose to keep their diagnosis to themselves because they fear losing their job or facing difficulties in obtaining employment.
However, there are also reasons that support being open about one’s diagnosis. Heiding continuously the condition from others can be mentally exhausting and often not possible. Being open and honest about one’s challenges can be relieving.
Without knowledge of the diagnosis, it is impossible to seek necessary treatment. Colleagues and supervisors who might be aware of the diagnosis are more likely to provide understanding and support for your condition. In larger companies, there is often an option to approach the works council or occupational health service in strict confidence.
If you’re concerned about your mental health condition, feel free to contact us on WhatsApp


